There are approximately 30 trillion cells in the human body, and close to 40 trillion bacterial organisms may live within and between those cells. While most people don't see or feel these microorganisms, scientists have proven that they are an essential part of life that can either support bodily health or increase the risk of disease and illness.
Many of these bacterial organisms exist in the vagina, and women can experience bacterial vaginosis, otherwise known as BV, when there is an imbalance between certain types of bacteria. This is often a silent condition that many women don't realize they have, but it can still increase their risk of developing sexually transmitted infections and diseases. Sexually active women under the age of 45 are most at risk, but it's important for all women to understand what bacterial vaginosis is and what symptoms it may present.
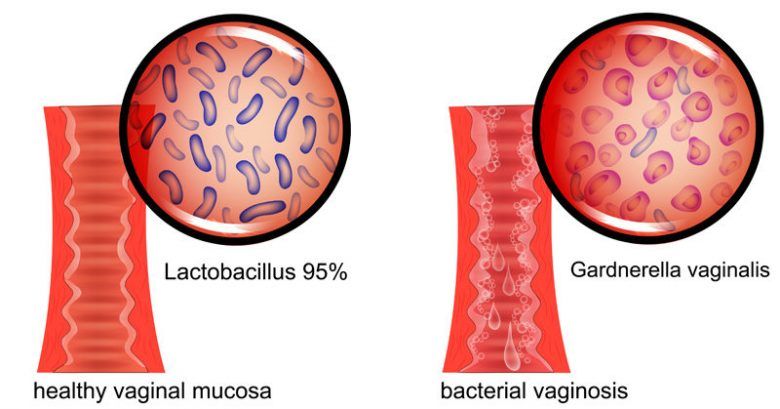
Bacterial vaginosis is caused by changes in the balance of the vaginal flora (imbalance between a "good" Lactobacilli bacteria in the vagina and other "bad" bacteria, such as Gardnerella vaginalis).

Normal Vaginal Flora (left) vs Bacterial vaginosis (right).
Other names: Bacterial Vaginitis, BV, Vaginal Bacteriosis

What Is Bacterial Vaginosis?
The professional version of the Merck Manual describes bacterial vaginosis as "vaginitis due to a complex alteration of vaginal flora." To gain a full understanding of this definition, it's helpful to elaborate on the meaning of vaginitis and the vaginal microbiome, which contains the vaginal flora.
Vaginitis is any type of inflammation in the vagina or vulva. While vaginitis can occur in females of all ages and for various reasons, bacterial vaginosis rarely impacts young girls or women who are not sexually active. This form of inflammation is caused by an imbalance in the microorganisms inhabiting the vagina, which are referred to by Merck as flora. Medical researchers are still uncertain why this imbalance typically occurs only in women who are sexually active and within their childbearing years.
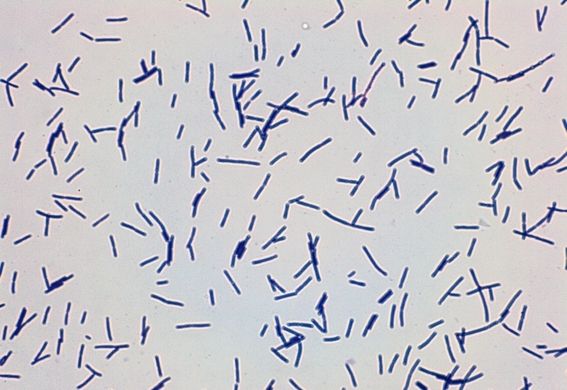
In the June 2012 issue of the Annual Review of Microbiology, researchers discussed developments in scientific understanding of the vaginal microbiome and the related condition of bacterial vaginosis. They revealed that Lactobacillus bacteria dominate the vaginal cavity in healthy women, but there are also other types of microbes commonly found in the vagina.
Some types of bacteria in the vaginal microbiome support human health. For instance, they often kill harmful bacteria because they see those bacteria as competitors for food. When these supportive bacteria dominate the vaginal cavity, women are at reduced risk for a variety of diseases and infections.
When there is disruption in the vaginal microbiome and harmful bacteria are present in large numbers, bacterial vaginosis is the most likely result. The supportive Lactobacillus bacteria are outnumbered, and opportunistic infections are more likely to take hold. This includes many organisms associated with sexually transmitted diseases.
While bacterial vaginosis was once thought of as a collection of symptoms, researchers are now gaining deeper insight into the microbes that help maintain vaginal health. Ongoing research will reveal even more information regarding the various microbiota found in this area of the female body.
Causes

Bacterial vaginosis is caused by changes in the balance of microorganisms in the vagina. Healthy women without BV are mostly populated by Lactobacilli bacteria. These bacteria are associated with positive vaginal health. Gardnerella Vaginalis and other harmful bacteria are commonly found in abundance in women who test positive for BV (the so-called BV-associated bacteria (BVAB), such as Prevotella spp, Atopobium vaginae, Mobiluncus spp, etc.). The symptoms of bacterial vaginosis are caused directly by the higher concentration of these harmful bacteria and limited activity of more beneficial bacteria.
Facts About Bacterial Vaginosis
- More than 20 million women are infected with bacterial vaginosis in the United States alone.
- More than 80 percent of women diagnosed with BV have no noticeable symptoms.
- Sexual abstinence is the best way to prevent bacterial vaginosis.
- African-American women are twice as likely to contract bacterial vaginosis.
- It is believed that a bacteria known as G. vaginalis is the most common culprit in the outbreak of BV.
- More than 50 percent of women who experience bacterial vaginosis will relapse within six months of treatment.
- Research has shown a connection between BV and personal hygiene habits, including changing underwear and bathing daily.
Signs & Symptoms of Bacterial Vaginosis
Up to 75 percent of bacterial vaginosis sufferers experience no noticeable symptoms. Most of these women learn that they have the condition when they're diagnosed during a routine vaginal examination. The prevalence of the condition is likely much higher than we know today because many women are likely unknowingly infected and are never diagnosed through routine examinations.
Women who do present symptoms are likely to experience one or more of the following signs of BV:
- Off-white or grayish vaginal discharge
- Fish-like vaginal odor
- Irritation or itching around the vaginal opening
- Burning with urination
Some women may notice the foul odor of BV just before or during their period. The odor may also become stronger after sexual intercourse.
Pictures
BV Risk Factors
While there is no clear understanding of what causes an imbalance in vaginal flora, researchers have studied the trends to establish a list of factors believed to increase a woman's risk for developing bacterial vaginosis. Not all of these potential causes of BV are avoidable for all women, but it's important for every sexually active woman to understand her risk factors.
Multiple or New Sexual Partners
Research has shown that approximately 34 percent of women in monogamous relationships test positive for bacterial vaginosis, but the rate goes up to more than 60 percent for women who entertain multiple sexual partners. It's also believed that women are at greater risk for contracting the condition when they start interacting with a new sexual partner, so the risk can multiple with each new partner introduced.
While it is generally believed that men cannot contract BV from infected women, some studies have found G. vaginalis, mycoplasma hominis and other bacteria associated with BV in the urethra of males. This suggests that males may pass these harmful bacteria to their female sexual partners. This would explain why most women display symptoms of BV soon after they make sexual contact with a new partner.
Frequent Douching
A study published in the May 2008 issue of the American Journal of Epidemiology tested more than 3,500 women for BV every quarter for one year. The results confirmed that women who douche are more likely to suffer from bacterial vaginosis. It is believed that the risk goes up with greater frequency of douching, and this is likely due to washing out beneficial bacteria in the process of cleansing the vagina.
Lack of Condom Use
A case-crossover analysis of research into the connection between condoms and bacterial vaginosis found that women who consistently use condoms do have a reduced risk of developing the condition. This validates what medical professionals have believed for many years and gives all women who aren't exclusive to one sexual partner good reason to always use condoms.
Lesbian Sexual Contact
Bacterial vaginosis can easily spread between women. One of the more prominent studies took vaginal samples from more than 100 women who identified as lesbians, including 21 lesbian couples. Approximately 29 percent of all participants tested positive for BV, and approximately 73 percent of those diagnosed with the condition had partners who also tested positive.
It's likely that women are at greater risk for developing BV due to direct vaginal contact and the transfer of bacteria, but there is also some research showing that women can contract the condition after performing oral sex on an infected woman. One study found that more than 65 percent of women actively performing oral sex on other women were positive for BV, but lesbian participants who did not practice oral sex all tested negative.
Further research is needed to fully understand how BV is transferred between women, but in the meantime, women who are sexually active should ask for BV testing during their routine vaginal examinations due to their heightened risk.
Wearing an IUD
A study published in the journal Sexually Transmitted Diseases in 2013 found that women who chose the intrauterine device or IUD as a form of sexual protection were more likely to experience bacterial vaginosis at some point. The research included 153 women who tested negative for BV at the beginning of the study. More than 50 percent of those women chose the IUD for protection, and approximately 37 percent of them experienced at least one BV infection. Fewer than 20 percent of women who chose other forms of protection experienced BV during the study.
It's possible that irregular bleeding may increase the risk of contracting BV while wearing an IUD. It's not currently understood why the IUD increases the risk of this condition, but it's something for all women to consider when selecting their preferred form of sexual protection.
Diagnosis
Diagnosis of bacterial vaginosis requires a pelvic examination and microscopic analysis of fluids collected during the exam. The doctor may notice the characteristic fish-like odor of the vagina as well as swelling and sensitivity inside the vagina. These are signs of a vaginal infection, but it doesn't rule out sexually transmitted diseases, which often present with the same symptoms.

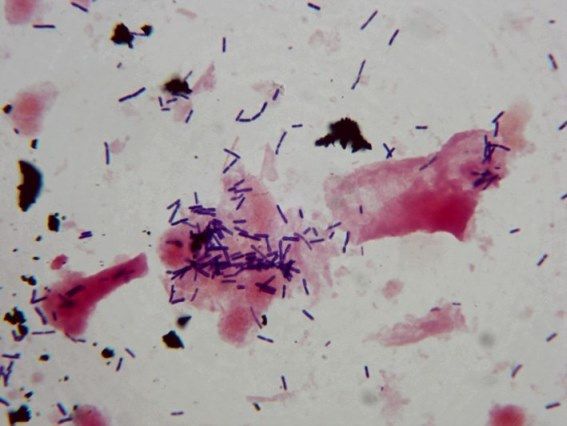
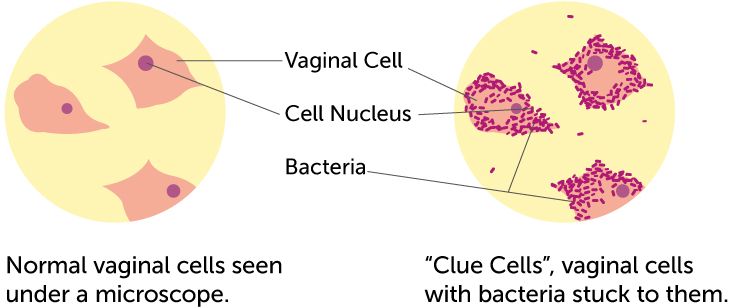
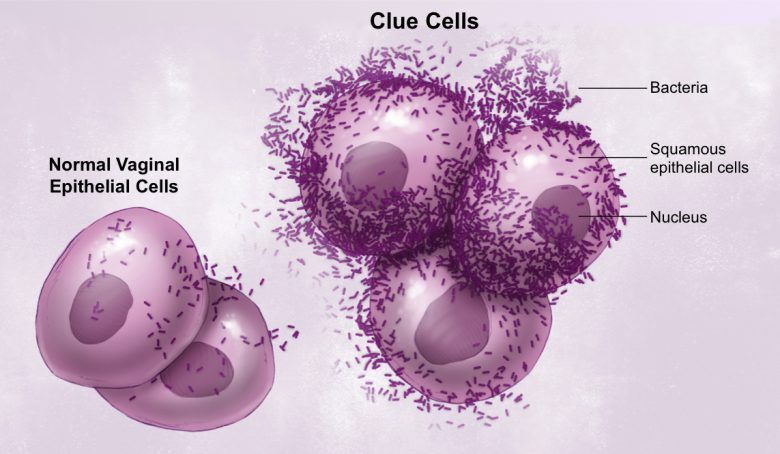
For a specific diagnosis of BV, a gynecologist or another medical professional will look at a sample of vaginal fluid under the microscope to identify the presence of clue cells. Along with white blood cells and signs of bacteria, the clue cells often hint to a positive BV test. A high PH level is also detected in most bacterial vaginosis cases.
For sexually active women, the medical professional may also test for a variety of sexually transmitted diseases. If no other diseases are detected and the microscopic analysis of vaginal fluid contains signs of bacterial vaginosis, this is likely the final diagnosis.
Treatments
Even if symptoms of bacterial vaginosis are mild or unnoticeable, it's important for women to complete the full treatment recommended by their medical providers. This will lower the risk of complications while reducing the woman's chance of relapsing with a repeat infection of BV in the future.
Treatment recommendations can vary depending on the overall health of the woman, but most will include one of the following antibiotics:
- Metronidazole – 500 mg pills or topical gels
- Clindamycin creams, ovules or pills
- Tinidazole – 1-2 grams daily
The CDC also recommends the following interventions while BV treatment is administered:
- Abstinence from alcohol consumption
- Abstinence from sexual contact or strict condom usage
- No douching or intense internal washing
Bacterial Vaginosis Treatment Guidelines
| Recommended Regimen: | |||
| Antibiotic: | Dose: | Route of medication administration: | Course of medication: |
| Metronidazole | 500 mg | orally | twice a day for 7 days |
| OR | |||
| Metronidazole gel 0.75% | one full applicator (5000 mg) | intravaginally | once a day for 5 days |
| OR | |||
| Clindamycin cream 2% | one full applicator (5000 mg) | intravaginally | once a day at bedtime for 7 days |
| Alternative Regimen: | |||
| Antibiotic: | Dose: | Route of medication administration: | Course of medication: |
| Tinidazole | 2000 mg | orally | once daily for 2 days |
| OR | |||
| Tinidazole | 1000 mg | orally | once daily for 5 days |
| OR | |||
| Clindamycin | 300 mg | orally | twice daily for 7 days |
| OR | |||
| Clindamycin ovules | 100 mg | intravaginally | once at bedtime for 3 days |
| Warning! Use of condoms and vaginal contraceptive diaphragms within 72 hours following treatment with clindamycin ovules is not recommended, becouse clindamycin ovules use an oleaginous base that might weaken latex or rubber products. | |||
Medications for Bacterial Vaginosis (BV)
| Drugs Used to Treat Bacterial Vaginosis (BV) | |
| Generics | Brand Names |
| metronidazole | Flagyl |
| metronidazole vaginal | MetroGel-Vaginal, Vandazole, Nuvessa |
| clindamycin | Cleocin (capsules, injection, granule for oral solution), Cleocin HCl (Oral), Cleocin Phosphate IV (Intramuscular, Intravenous), Cleocin Pediatric (Oral) |
| clindamycin vaginal | Cleocin Vaginal, Cleocin Ovules, ClindaMax, Clindesse, Clindesse Cream |
| clindamycin topical | Clindacin P, Cleocin T, Clindacin ETZ, Clindagel, Evoclin, Clindacin PAC |
| tinidazole | Tindamax, Fasigyn |
| acetic acid vaginal | Acid Jelly, Fem pH, Relagard, Aci-Jel, Acidic Vaginal Jelly, Bidette, Feminique, Massengill Douche |
| secnidazole | Solosec |
Are Probiotics Effective for Bacterial Vaginosis Treatment?
Since BV is caused by a reduction in the presence of Lactobacilli bacteria in the vagina, it makes sense that supplementing with this bacterium may help in the treatment and prevention of the condition. There has been some scientific research into this theory, but the results have caused some controversy.
For instance, one study found that treating women with BV with Lactobacillus acidophilus bacteria injected directly into the vagina for up to 12 days was effective at reversing the bacterial imbalance. This cured the condition for some women and was proven effective at reducing the rate of recurring infections. Oral probiotic supplements were also proven effective for treatment and prevention, but women needed to continue the supplement for two months to get those results.
While there have been studies that dispute the effectiveness of probiotic supplements for the treatment or prevention of bacterial vaginosis, there is growing support for the use of probiotics at least as a preventative measure. Some of the more effective bacteria to include in an effective supplement include:
- Lactobacillus acidophilus
- Lactobacillus rhamnosus GR-1
- Lactobacillus fermentum RC-14
Outlook
According to the Harvard Medical School, the outlook for women suffering from bacterial vaginosis is excellent. While there is some risk of complication for women who aren't properly treated for the condition, those who do receive treatment typically recover quickly with mild to moderate discomfort.
There is a risk of recurrent BV. Up to 30 percent of sufferers will experience recurrence of symptoms within three months, and at least one study has shown that more than half of all women diagnosed will have a repeat occurrence at some point. Women can reduce their risk of recurring infections by limiting their risk factors and having routine pelvic examinations to catch signs of bacterial imbalance early. Daily probiotic supplementation may also help.
Bacterial Vaginosis Complications
The imbalance in vaginal bacteria leaves women at higher risk for contracting other diseases. This is likely due to the reduced presence of healthy bacteria that would normally help eliminate harmful microbes before they can develop into an infection or disease.
Some of the most common infections for women to contract when BV isn't quickly and properly treated include:
BV may also increase the risk of infection during a surgery and often interferes with in-vitro fertilization treatments.
Prevention
The first step to preventing bacterial vaginosis is to acknowledge the risk factors and work toward eliminating or at least limiting those risks. For instance, many women have given up douching and avoid excessive internal washing since those behaviors are associated with the reduction of beneficial bacteria in the vagina. Many women are also supplementing with probiotics daily and taking out their IUDs.
It's also important to change underwear regularly, especially after intense exercise and other activities that may cause excessive vaginal discharge. Dedication to quality personal hygiene and controlling the number of sexual partners entertained should keep many women from developing BV.
Bacterial Vaginosis in Pregnancy
Due to the hormonal fluctuations that occur during pregnancy and the sexual encounters that lead to pregnancy, many women will develop symptoms of BV while carrying a baby. Research into the risks for pregnant women and their unborn babies is still in development, but there is enough evidence to acknowledge that BV may increase a mother's risk of the following:
- Low birth weight
- Miscarriage
- Premature membrane ruptures
- Pre-term labor
Most pregnant women aren't tested for bacterial vaginosis as a part of routine maternity care unless they display signs of the condition. Women can request this testing if they believe they're at high risk for the condition or just want to take extra precautions to protect their pregnancy.
Home Remedies
Women who don't want to take antibiotics or who suffer from recurrent bacterial vaginosis may try a variety of home remedies or natural treatments. Yogurt is often used because it naturally contains beneficial bacteria needed to keep the body in balance. Not only are these bacteria helpful for the vaginal microbiome, but they can improve overall health by populating the gut microbiome with microbes that support life.
There is little scientific support for other home remedies for bacterial vaginosis, but some of the natural treatments commonly used today include:
- Garlic supplements
- Boric acid capsules
- Vaginal washing with hydrogen peroxide
- Tampons soaked in diluted tea tree oil
It's important to note that there is some risk with some of these alternative treatments for BV. Women should test tea tree oil and all other essential oils on a small patch of skin before placing it inside their vagina. Excessive internal washing is considered a risk for the development of bacterial vaginosis, so hydrogen peroxide washing daily isn't always productive.
FAQs
How does bacterial vaginosis spread?
There is a strong connection between BV and sexual activity, especially between two women. Research has shown that some men may carry harmful bacteria that can lead to bacterial vaginosis in future sexual partners, but men don't present symptoms of the condition and aren't typically treated. BV isn't considered a sexually transmitted disease because there are many other factors that could cause an imbalance in bacteria within the vagina.
Can women contract BV from toilet seats?
The average toilet seat contains about 50 bacteria per square inch, but it's not likely to include the type of bacteria that can cause BV. You're more likely to spread staph or catch a cold or the flu if you touch a toilet seat without washing your hands immediately after.
Can virgins get bacterial vaginosis?
It's possible for females of all ages to suffer from an imbalance in vaginal flora. BV is typically found in sexually active women of child-bearing age, and that rules out most children and young girls. There are other potential causes of BV that don't involve sex, so some virgins are diagnosed with this condition. It's also important to note that oral sex may lead to BV even if a girl hasn't had sexual intercourse.
What should a woman do if she thinks she has BV?
It's important for all women to see their gynecologist or another medical professional when they first notice potential signs of bacterial vaginosis. A pelvic examination is needed to determine the cause of the symptoms, and women are at heightened risk of HIV and many other diseases if BV is left untreated.
Can a man give a woman bacterial vaginosis?
Research has shown that men can harbor bacteria that are harmful to the vagina. Men won't show symptoms of BV and aren't commonly treated, but it's possible that they can transfer harmful bacteria to their sexual partners. This is why it's important for men to wear condoms if they aren't in a monogamous relationship. Women should insist on strict condom usage if they have multiple partners or when having sex with a new partner. The early signs of BV typically start soon after sexual contact is made with a new partner.
Why are lesbians more likely to get BV?
While the bacteria found in a woman's vaginal microbiome is often unique, it's common for female lovers to share many bacterial qualities. This is likely due to direct vaginal touching with fingers and other body parts, which allows the transfer of bacteria from woman to woman. If one woman has an abundance of harmful bacteria, it's likely to transfer to her lover's vagina during intimate moments.
Sources
- https://www.cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm
- https://www.cdc.gov/std/tg2015/bv.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3249696/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5621139/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5558670/
- https://hospitals.jefferson.edu/diseases-and-conditions/bacterial-vaginosis.html
- http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.486.1715&rep=rep1&type=pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2574994/
- https://www.ncbi.nlm.nih.gov/pubmed/17917605
- https://academic.oup.com/cid/article-abstract/21/6/1402/274703
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285477/
- https://www.uofmhealth.org/health-library/hw3367
- https://www.ncbi.nlm.nih.gov/pubmed/17633390
- https://www.health.harvard.edu/a_to_z/bacterial-vaginosis-gardnerella-vaginitis-a-to-z