What Is Trichomoniasis (Trich)?
Trichomoniasis, more commonly referred to as trich, is a sexually transmitted infection, or STI. As with many other infectious diseases, it's possible to be infected with trich yet display no outward symptoms. According to the U.S. Centers for Disease Control, or CDC, trich is the most common curable STI.
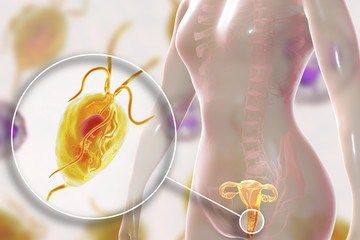
Trich is caused by a parasitic single-celled organism, or protozoan, named Trichomonas vaginalis. This species lives exclusively in the urogenital tracts, or reproductive and urinary systems, of human beings, but in the lab, scientists have observed it surviving for up to 24 hours in urine. Under the right conditions, it can travel readily from one individual to the next. The vast majority of cases involve infections of the lower genital tract body parts, including the vagina, cervix, vulva and urethra.

Trichomoniasis is caused by a parasitic protozoa Trichomonas vaginalis
Trichomoniasis Pictures
trichomoniasis discharge pictures
How Do You Get Trichomoniasis?
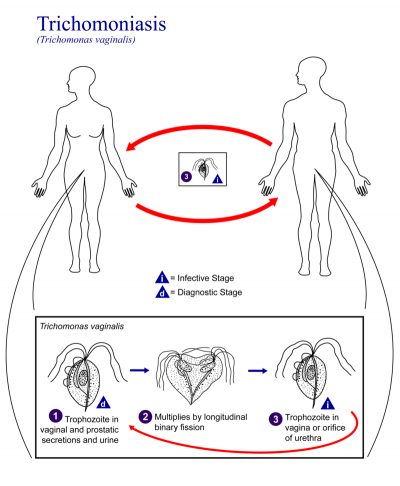
Trichomoniasis can potentially spread from one person to another via any form of sexual behavior that involves genital touching. This may include different types of sexual activities, but vaginal intercourse is the primary method of transmission.
As a parasite that resides in various parts of the urogenital tract, Trichomonas vaginalis can be spread with or without an exchange of internal fluids, such as semen and precum. Genital-to-genital contact, such as when people have nonpenetrative sex, can spread the infection.
In some cases, this STI propagates when infected individuals touch their genitals and then touch a partner's genitals without washing their hands. Those who share unwashed sex toys can also spread trich. It's worth noting that Trichomonas vaginalis parasites don't propagate through conventional forms of contact, such as holding hands, sneezing or sharing foods.

Risk Factors
Certain population groups are more at risk of coming down with trichomoniasis. For instance, women, who can develop infections in their urethras or vaginas, are at a greater risk than men, who only develop infections in the urethra.
Although millions of women aged from 14 to 49 come down with trich, being an older woman increases your risk. One 2011 study of more than 7,500 women between the ages of 18 and 89 from 28 states found that
- Females over 50 had the highest rate of infection, and women between 40 and 49 had the second-highest,
- As with other STIs, individuals who faced poverty, lack of education and unemployment were more likely to have trich,
- In jails, the infection rate was around 22.3 percent, and
- In the Southeast U.S., which typically skews poorer than other areas, the trich rate was the highest of all U.S. regions at 14.4 percent.
Being sexually active increases the likelihood that you might have trich, and being sexually active as a member of an already at-risk group or community, such as African-American individuals, raises it even further. Other risk factors include
- Being sexually active with multiple partners,
- Douching, which can heighten your trich risk by eliminating some of the normal, healthy vaginal bacteria that might otherwise prevent an infection,
- Abusing drugs or alcohol to the point where you might engage in dangerous behaviors,
- Being sexually active without using protection, such as a condom, and
- Having a history of other STIs or prior trich infections.
Facts
Trichomoniasis infections impact millions of people each year. In 2015 alone, around 122 million cases were reported, and at any given moment in the U.S., approximately 3.7 million people have trich. By some estimates, about 180 million women worldwide may have this STI. Other figures claim annual infection rates of 160 million people.
A pioneering French bacteriologist named Alfred François Donné, who also identified leukemia, first identified the Trichomonas vaginalis protozoan in the 1830s. It would take until 1916, however, before researchers first recognized the connection between the organism and the trichomoniasis STI. Today, scientists have sequenced the organism's DNA and discovered that most specimens fall into one of two varieties.
Signs and Symptoms
Trichomoniasis is unique because the vast majority of infected individuals never show symptoms. For the 30 percent who do start developing signs, symptoms might not appear immediately: It can often take between 5 and 28 days before you notice that something is wrong. The delay between an initial infection and the onset of problems may be even longer, but most people start to feel it within a month. Your symptoms may also worsen and recede at different times.
Symptomatic Gender Differences
Women and men don't always experience the same trich symptoms. This disparity may make it difficult to discern whether you and a partner are suffering from the same STI:
 In females, trichomoniasis can make the genitals burn, itch or feel sore. About two percent of women develop a reddened, swollen cervix, also known as "strawberry cervix," or colpitis macularis. It may become uncomfortable to urinate. You might also notice changes in your vaginal discharge. For instance, some sufferers experience abnormal volumes of discharge or notice that the consistency of their discharge has become unusually frothy, runny or thick. This substance may range in color from clear or white to yellowish or greenish, and it often emits an uncharacteristic, unpleasant odor commonly described as "fishy" or "musty." In some cases, the vaginal discharge will contain blood.
In females, trichomoniasis can make the genitals burn, itch or feel sore. About two percent of women develop a reddened, swollen cervix, also known as "strawberry cervix," or colpitis macularis. It may become uncomfortable to urinate. You might also notice changes in your vaginal discharge. For instance, some sufferers experience abnormal volumes of discharge or notice that the consistency of their discharge has become unusually frothy, runny or thick. This substance may range in color from clear or white to yellowish or greenish, and it often emits an uncharacteristic, unpleasant odor commonly described as "fishy" or "musty." In some cases, the vaginal discharge will contain blood.- In males, trichomoniasis infections can be associated with a burning sensation that typically follows ejaculation or urination. The urethra, or inside of the penis, may also itch, feel irritated or produce abnormal discharge.
One common symptom that impacts both sexes is the fact that trich might make sexual activity feel distinctly uncomfortable. Regardless of their sex, infected individuals can experience symptoms of varying severity, with some people reporting only mild discomfort and others noting that their genitals become extremely inflamed and outright painful. Some people report feeling the urge to urinate more often than they normally would.
Not every STI carrier has all of the symptoms. You and your partner might not even experience the same issues. One important thing to remember is that because a parasite causes trich, it can have a long-term impact. If left untreated, the infection may last for years even if it seems to go away periodically.
Many of the symptoms associated with trichomoniasis also occur in patients with other STIs, such as yeast infections and urinary tract infections, or UTIs. This unfortunate reality can make it difficult to distinguish between trich and other diseases, so professional testing and diagnosis are essential.
Causes
Infection by Trichomonas vaginalis is the sole cause of trichomoniasis. Because men typically experience fewer symptoms, they may fail to seek treatment, and healthcare professionals might not diagnose them. Unprotected sexual activity with an infected individual is the primary cause of infection.
Testing and Diagnosis
Thanks to years of study, there are various testing options for people who think that they might have trich. Since these diagnostic techniques are low-cost, minimally invasive and commonplace, it's definitely worth taking the time to get tested.
As with many STIs, trich diagnosis begins with an examination. Your caregiver may perform a visual inspection of your genitals to eliminate other common infections before deciding what to test for. In many cases, you'll be tested for multiple things to increase the accuracy of the diagnosis. After that, you might be asked to provide a urine sample for lab examination. Doctors can also use a cotton swab to collect cell samples from your genitals.
Once they've taken a sample, your caregiver will typically send it to an independent lab. By growing the sample cells in a sterile culture, technicians can determine what exactly they are and help confirm the diagnosis. Other techniques include examining the sample under a microscope, which is more affordable yet less accurate than the culture option. The costliest, most sensitive method is nucleic acid amplification testing, or NAAT, which involves hunting for specific genetic materials and byproducts associated with the Trichomonas vaginalis organism.
Prevention
Not having sex or sticking to one partner are good ways to prevent the spread of infection. Since these options are unrealistic for many people, however, it's important to use protection. Trichomoniasis can't spread through physical barriers, so wearing a male or female condom can make it safer to have intercourse with an infected individual. In most cases, it's wise to avoid sharing sex toys.
Getting tested at the first sign of symptoms is also another critical aid in prevention. The less time you spend engaging in sexual activity without knowing that you're infected or whether your partner is infected, the higher the chances are that you won't play a role in spreading trich. Also be aware that since trich tests aren't typically part of physical exams, it's up to you to request one if you suspect something.
Treatment
Although trich is extremely common, it's also extremely easy to deal with. There are a number of cures, so it's important to talk to your caregiver about what's best for you.
Treatment for Couples
Treating your partner is just as important as getting treated yourself. Even if you get cured, you may become reinfected down the line by a sexual partner who continues to harbor the STI. In most cases, doctors will recommend that you and your partner undergo treatment at the same time.
Antibiotics
The vast majority of people with trich get cured by taking an oral dose of the medication metronidazole, which may be available under various brand names. This remedy solves 95 to 97 percent of cases, but it may not be appropriate for women in the early stages of pregnancy, individuals with diarrhea or some feeding-tube patients. While you typically only have to take metronidazole once, women who also have HIV may be placed on a longer regimen by their doctors.
Metronidazole may cause limited adverse effects, such as hypersensitivity, darkened urine or vomiting. Pregnant women and those likely to experience negative drug reactions may be given another antibiotic named tinidazole as an alternative treatment. With both antibiotics, it's important to avoid drinking alcohol.
It's also critical to understand that topical treatments typically don't work as well as oral antibiotics do. Since Trichomonas vaginalis is a microscopic organism, it can hide inside internal cavities, such as the Skene glands found on the vaginal wall near the end of the urethra. In other words, even if you apply an antibiotic cream liberally, you might not kill all of the protozoa that are causing your infection.
In a few cases, Trichomonas vaginalis can be resistant to antibiotics. These individuals may need to undergo further treatments at a later date if they become reinfected. This makes it imperative to consult with your primary doctor, gynecologist or internal medicine practitioner as a follow-up after your initial treatment.
Your Treatment Responsibilities
Medical treatments only work when patients follow them properly. Even though they're typically administered in single doses, the antibiotics that cure trich can require about a week to produce the desired impact. During this time, you should avoid all sexual activity, so ask your healthcare provider how long you'll need to wait before starting to have sex again. You also need to ensure that you follow the dosage instructions you receive.
Bear in mind that trich cures aren't permanent. To avoid reinfection by a new partner, always practice safe sex.
Medications for Trichomoniasis
| Drugs Used to Treat Trichomoniasis | |
| Generics | Brand Names |
| metronidazole | Flagyl, Flagyl 375, Flagyl I.V. (Intravenous) |
| tinidazole | Tindamax |
Trichomoniasis Treatment Guidelines
| Recommended Regimen: | |||
| Antibiotic: | Dose: | Route of medication administration: | Course of medication: |
| Metronidazole | 2000 mg | orally | in a single dose |
| OR | |||
| Tinidazole | 2000 mg | orally | in a single dose |
| Alternative Regimen: | |||
| Antibiotic: | Dose: | Route of medication administration: | Course of medication: |
| Metronidazole | 500 mg | orally | twice a day for 7 days |
T. vaginalis & HIV infection
| Recommended Regimen for Women with HIV Infection: | |||
| Antibiotic: | Dose: | Route of medication administration: | Course of medication: |
| Metronidazole | 500 mg | orally | twice daily for 7 days |
Outlook
For most people, trich has a largely favorable prognosis, or expected development. Those who get treated are usually able to move on with their lives without having to permanently give up sexual activity or anything else that they enjoy.
Complications
Not all trich sufferers get away with simply taking antibiotics. For instance, people who don't know they have the disease might fail to get treatment or also carry other STIs that increase their likelihood of medical problems.
Some potential issues to consider include the following:
- Pregnant women with trichomoniasis are at risk of giving birth to premature infants or infants with abnormally low birth weights of less than 5.5 pounds.
- Trich infections are commonly linked to heightened risks of HIV transmission and infection. This is especially true when genital swelling is present because the inflammation makes it easier for the HIV to get past your skin barrier.
- Women who don't get treated may develop persistent vaginitis, or irritation of the vagina or vulva.
- Males with trich may be at higher risk of diseases like prostatitis, urethritis and chronic prostate inflammation that can cause prostate cancer.
- Trich infections may be associated with concurrent infections involving HPV, or human papillomavirus, which causes cervical cancer.
FAQs
Can't my doctor diagnose me just by looking?
Trich symptoms are too common to serve as the sole basis for accurate diagnosis. Lab testing is a must no matter your gender or perceived symptoms.
Why did I get trich again even though my partner and I both took antibiotics?
Approximately 20 percent of trich patients get the STI again with three months of their first treatment. Such outcomes can be due to poor sexual hygiene or a failure to follow the prescription regimen properly, but they may also be the result of having an antibiotic-resistant trich strain.
Can I give trich to my baby if I'm pregnant?
In some extremely rare cases, mothers might pass trich on to their babies during the childbirth process. Fortunately, there are trich treatments that are safe to use during pregnancy.
Can I test myself for trich without going to the doctor?
There are some commercially available STI test kits that you can use to collect your own sample from home before mailing it to a lab. Since you don't know whether you also have other STIs, however, consulting with a professional is usually the safest bet.




 In females, trichomoniasis can make the genitals burn, itch or feel sore. About two percent of women develop a reddened, swollen cervix, also known as "strawberry cervix," or colpitis macularis. It may become uncomfortable to urinate. You might also notice changes in your vaginal discharge. For instance, some sufferers experience abnormal volumes of discharge or notice that the consistency of their discharge has become unusually frothy, runny or thick. This substance may range in color from clear or white to yellowish or greenish, and it often emits an uncharacteristic, unpleasant odor commonly described as "fishy" or "musty." In some cases, the vaginal discharge will contain blood.
In females, trichomoniasis can make the genitals burn, itch or feel sore. About two percent of women develop a reddened, swollen cervix, also known as "strawberry cervix," or colpitis macularis. It may become uncomfortable to urinate. You might also notice changes in your vaginal discharge. For instance, some sufferers experience abnormal volumes of discharge or notice that the consistency of their discharge has become unusually frothy, runny or thick. This substance may range in color from clear or white to yellowish or greenish, and it often emits an uncharacteristic, unpleasant odor commonly described as "fishy" or "musty." In some cases, the vaginal discharge will contain blood.