Contents
- 1 What Is Pelvic Inflammatory Disease?
- 2 Causes of Pelvic Inflammatory Disease
- 3 Facts Women Should Know About Pelvic Inflammatory Disease
- 4 Signs and Symptoms of Pelvic Inflammatory Disease
- 5 Risk Factors for Pelvic Inflammatory Disease
- 6 Diagnosis of Pelvic Inflammatory Disease
- 7 What Are the Treatments for Pelvic Inflammatory Disease?
- 8 What Is the Outlook for Women With PID?
- 9 Complications of PID
- 10 PID and Female Infertility
- 11 Prevention of PID
- 12 Frequently Asked Questions About Pelvic Inflammatory Disease
- 12.1 Can a Pap test detect PID?
- 12.2 Are natural home remedies for PID pain used?
- 12.3 Can PID be cured?
- 12.4 Is it possible for PID to come back?
- 12.5 Does taking oral contraceptives lower my risk of developing PID?
- 12.6 Can women who only have sex with women develop PID?
- 12.7 When should I see a doctor?
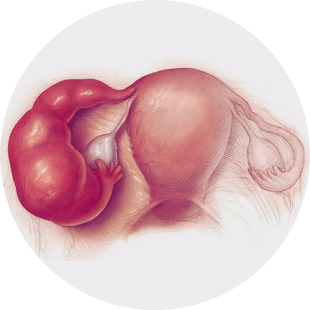
What Is Pelvic Inflammatory Disease?
Pelvic inflammatory disease, often referred to as PID, is an infectious and inflammatory condition involving one or more of the female reproductive organs. PID infections typically occur in three stages. The cervix, which is the opening of the womb, is normally the first area affected. This is followed by the lining of the uterus known as the endometrium and then the fallopian tubes.
Causes of Pelvic Inflammatory Disease
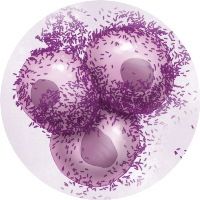
PID occurs when there is an infection in the upper genital tract. The infection typically starts in the vagina or cervix and travels into the womb, ovaries, and fallopian tubes. According to the Centers for Disease Control, anywhere from one-third to half of all PID cases are caused by sexually transmitted infections, primarily chlamydia and gonorrhea. Chlamydia infections account for roughly 50 percent of sexually acquired PID infections while gonorrhea infections account for approximately 25 percent. Although not as common, Mycoplasma genitalium has also been linked to pelvic inflammatory disease.
In some women, the infection occurs when bacteria normally found in the vagina make their way into the upper reproductive organs. This is most likely to occur when there has been damage to the womb, such as during childbirth or a miscarriage, or following an invasive procedure, such as an examination, insertion of an intrauterine contraceptive device, or an abortion. In rare cases, the infection can occur following a burst appendix or bowel infection.
Facts Women Should Know About Pelvic Inflammatory Disease
Although the number of PID diagnoses has decreased over the past decade, it is still a common infection among sexually active women of reproductive age. According to the 2013-2014 National Health and Nutrition Examination Survey, 4.4 percent of sexually active women in the U.S. between the ages of 18 and 44 reported having had PID at least once during their lifetime. That translates to approximately 2.5 million women. PID is often considered a silent epidemic since many women do not experience symptoms or have symptoms so mild that they do not seek diagnosis and treatment.
Signs and Symptoms of Pelvic Inflammatory Disease
The symptoms of PID can range from mild to severe. Diagnosis can be complicated by the fact that symptoms are often nonspecific and may mimic other conditions of the genitourinary and gastrointestinal tracts. Common symptoms include:
- mild to severe lower abdominal pain,
- abdominal and pelvic tenderness,
- increased or unusual vaginal discharge,
- heavy or irregular menstrual bleeding,
- painful intercourse and urination, and
- fever.
Risk Factors for Pelvic Inflammatory Disease
A number of factors are associated with an increased risk of developing PID, including:
- being sexually active and under the age of 25,
- not using a condom during sex,
- engaging in sex with multiple partners or having sex with someone else who has had multiple partners, and
- having a prior history of sexually transmitted infections or PID.
According to some experts, there is a slightly increased risk of developing PID during the first three weeks following the insertion of an intrauterine contraceptive device. Regular douching may also increase the risk by altering the bacterial balance of the vagina and masking potential symptoms.
Diagnosis of Pelvic Inflammatory Disease
An initial diagnosis of PID is typically based on the patient’s signs and symptoms. A pelvic exam will normally be performed to check for abdominal, uterine, and pelvic organ tenderness. In most cases, additional tests are performed to confirm the diagnosis and identify the underlying source of the infection.
Swabs and Cultures
The doctor may use a cotton swab to obtain samples from the cervix and vagina. The sample is cultured and examined under a microscope to identify the specific organism causing the infection.
Blood and Urine Tests
Blood and urine tests will be used to rule out urinary tract infections, ectopic pregnancy, and other potential causes of the symptoms. The blood panel will also typically include a complete blood count, sedimentation rate, and C-reactive protein. The complete blood count will normally show an elevated number of white blood cells, which is an indication of infection, and the sedimentation rate and C-reactive protein may be elevated due to the inflammation. Since pelvic inflammatory disease is often associated with sexually transmitted infections, such as gonorrhea and chlamydia, the doctor may also perform screenings for these conditions as well.
Ultrasound
A pelvic or transvaginal ultrasound, which is a painless procedure that uses sound waves to create images of the internal organs, may be used to rule out other potential causes of the pain.
Laparoscopy
A laparoscopy may be performed to check the pelvic organs for signs of infection and scar tissue. The procedure is performed by inserting a thin, lighted scope through a small incision in the abdomen.
MRI or CT Scan
Although not typically used to diagnose pelvic inflammatory disease, an MRI or CT may be performed in cases where symptoms do not improve with treatment or if an ultrasound shows a mass or abscess that requires further evaluation. Both procedures are noninvasive, painless, and allow the doctor to visualize the internal structures of the abdomen.
What Are the Treatments for Pelvic Inflammatory Disease?
If diagnosed and treated early, most cases of PID can be cured. Even if you have only one or two minor symptoms, you should see a doctor immediately to reduce the risk of long-term damage and infertility.
Antibiotics
The primary treatment for PID is antibiotics. Depending on your symptoms and medical history, the doctor may prescribe medication before all of the lab tests are completed and then adjust the medication as necessary to better target the specific infection. To avoid a recurrence of the infection, it is important to complete the full course of antibiotics even if you start to feel better. In severe cases, hospitalization and intravenous antibiotics followed by oral antibiotics may be required. It is common for the infection to be caused by more than one type of bacterium, so multiple types of antibiotics may be prescribed.
Treatment for Sexual Partners
Since PID is frequently caused by sexually transmitted infections, it is important that any sexual partners that you have had within the past 60 days be tested and treated as necessary. It is possible for someone to be infected yet not experience any symptoms, so it is important for them to consult their health care provider.
Temporary Abstinence
To reduce the risk of reinfection, women with PID should avoid sexual intercourse until they and their partners have completed treatment and been advised by a doctor that it is safe to resume. The length of time that you should abstain can vary based on the type of treatment.
Surgery
Although rare, surgery may be required in cases where there is an abscess or to remove scar tissue or adhesions.
Follow-up
Follow-up care is vital to ensure that the treatment is working and to reduce the risk of chronic pain, infertility, and other complications. Your doctor will likely want to see you within two to three days of starting antibiotic therapy to determine if the treatment is working or if an adjustment is needed based on the results of laboratory tests. Once you have had PID, you should have any further pelvic symptoms or fertility issues evaluated by your doctor or a reproductive health specialist.
What Is the Outlook for Women With PID?
Women who seek treatment promptly, complete the course of antibiotics as directed, and follow-up with their health care provider, often have no long-term side effects. Serious complications can arise, however, if the infection goes untreated or if treatment is delayed.
Complications of PID
Abscesses, which are pockets of pus, can develop around the ovaries or fallopian tubes. The infection can spread through the lower belly in a condition known as pelvic peritonitis. PID can also cause inflammation around the outside of the liver. In some women, pelvic inflammatory disease can cause chronic pain, which can lead to depression, trouble sleeping, and otherwise make it difficult to carry out normal daily activities.
PID and Female Infertility
Many women do not realize that they have or have had pelvic inflammatory disease until they have trouble conceiving. As many as 1 in 8 women with a history of pelvic inflammatory disease experience difficulty getting pregnant, and the risk of infertility increases with each episode of PID or if treatment is delayed. The infertility occurs when abscesses or scar tissue make it difficult for the eggs to pass from the fallopian tubes into the uterus. A single episode of PID can increase the risk of tubal infertility 25 percent. The risk increases to 75 percent following three or more PID episodes. PID infections caused by gonorrhea are associated with a slightly higher risk of fallopian tube blockage.
Damage to the fallopian tubes also increases the risk of an ectopic pregnancy in which the fertilized egg begins to develop in the fallopian tube or elsewhere outside of the uterus. To prevent the fallopian tube from bursting, which can lead to severe internal bleeding, an ectopic pregnancy is treated by surgery to remove the egg or by medication to stop it from growing. The chances of experiencing an ectopic pregnancy increase approximately sevenfold following a single episode of pelvic inflammatory disease.
Prevention of PID
If you are sexually active, you can reduce your risk of developing pelvic inflammatory disease by taking the following steps:
- Limit your risk of contracting sexually transmitted infections that can lead to PID by using a condom during every sexual encounter.
- Limit the number of partners with whom you have sex.
- Discuss sexual history before having sex with a new partner.
- Get tested for sexually transmitted infections on a regular basis if you engage in unprotected sex or have sex with someone who has had unprotected sex with another person.
- If you have any reason to suspect that you or your partner may have a sexually transmitted infection, get tested as quickly as possible. You should immediately abstain from having sex until you know the results of the tests and any necessary treatment has been completed.
- Don’t use douches.
Frequently Asked Questions About Pelvic Inflammatory Disease
Can a Pap test detect PID?
No. A Pap test is used to detect cancerous and precancerous cells in the cervix and will not detect pelvic inflammatory disease.
Are natural home remedies for PID pain used?
Q: I've heard it's sometimes advised to use turmeric powder. Is that true? Can he help?
A: "Curcumin is used as a remedy for the treatment and prevention of inflammatory diseases" (sourse), but, "in the gynecology and especially in the pelvic inflammatory disease the use of curcumin as a supplement has never been studied" (sourse).
Can PID be cured?
PID can be successfully treated and cured; however, treatment won’t reverse any damage that has already occurred to the reproductive tract, so prompt treatment reduces the likelihood of long-term complications.
Is it possible for PID to come back?
Resuming sexual activity too quickly after treatment can cause the infection to return, so it is important to find out from your doctor when it is safe to engage in sexual activity. PID and also recur if you develop a subsequent sexually transmitted infection. Women with a prior history of PID are also at higher risk of developing it again.
Does taking oral contraceptives lower my risk of developing PID?
There is some data showing that women taking oral contraceptives have one-third the risk of developing PID compared to women not taking contraceptives. It is important to note, however, that this information was collected in the 1970s, so it is not clear if today’s low-dose contraceptives offer the same type of protection. Women, regardless of contraceptive use, should still use condoms with new sexual partners to protect against sexually transmitted infections.
Can women who only have sex with women develop PID?
It is possible for women to transmit PID and sexually transmitted infections to other women. It is important to discuss sexual history with both male and female partners before engaging in sex.
When should I see a doctor?
You should contact your primary care doctor or seek emergency medical treatment if you experience:
- nausea and vomiting,
- a fever higher than 101°F, or
- severe lower abdominal pain.
Foul smelling vaginal discharge, bleeding between periods, and painful urination are common symptoms of sexually transmitted infections, which can lead to pelvic inflammatory disease if not treated promptly. If you experience these symptoms, you should abstain from sex and see your health care provider as soon as possible.