Unbearable burning and itching are the most unpleasant symptoms of the genitals - candidiasis or yeast infection. The disease is caused by a pathogenic yeast-like fungus of the genus Candida. In women the fungus affects the labia, the clitoris, and sometimes the gluteal and inguinal candidiasis is formed. Male yeast infection has another manifestation: the head of the penis is affected. Pathogens can also attack the rectum and oral cavity.

Contents
- 1 Frequency of Spreading
- 2 Forms of Candidiasis
- 3 Classification of Candidiasis (Yeast Infection)
- 4 Yeast Infection Symptoms
- 5 Candidiasis Infographics
- 6 What are the Causes and Risk Factors of Yeast Infection?
- 7 Consequences of Candidiasis
- 8 How is a Vaginal Yeast Infection Diagnosed?
- 9 Urogenital Candidiasis Treatment
- 10 How to Cure Yeast Infection: Therapy and Remedies
- 11 Methods for the Prevention of Urogenital Candidiasis
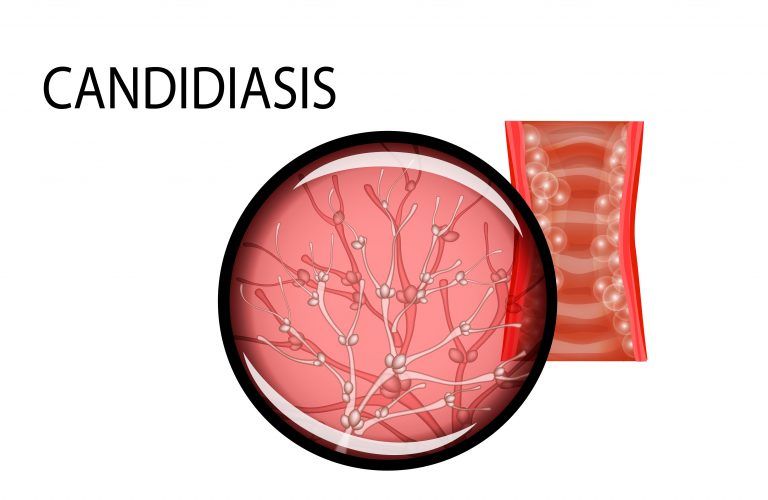
Candidiasis is a fungal infection due to any type of Candida (a type of yeast).
- When it affects the vagina, it is commonly called a yeast infection. Signs and symptoms
include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Less commonly the penis may be affected, resulting in itchiness. Very rarely, the infection may become invasive, spreading to other parts of the body.
- When it affects the mouth, it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing.
Frequency of Spreading
According to statistics, urogenital yeast infection is one of the most common infections of the genital tract. A third part of patients who have applied to medical institutions for vaginitis and other inflammations are diagnosed with candidiasis of the genital organs. This figure is even higher among women: two-thirds of the female population have become infected with thrush at least once in their lives. In most cases the patents subject to relapses.
According to statistics, there are 10 women to 1 infected man. This is because only 2% of men who have sex with an infected partner may get the fungus.
Today, asymptomatic forms of yeast infection are not rare. Atypical and chronic candidiasis are also common. Chronic course of the infection is observed not only due to poorly treated acute form of the disease, but also because of the resistance of the pathogen to the existing medical drugs.
Forms of Candidiasis
Depending on the spreading of the Candida fungus and the severity of infection, the following forms of the disease can be distinguished:
- Superficial. The fungus is formed only on the skin, nails and mucous membranes. This is one of the easiest manifestations of infection.
- Systemic. It affects not only the epithelium, but also internal organs: especially digestive and respiratory systems. Usually such a course of the infection is observed in patients with insufficient immune response: with AIDS or cancer.
- Acute. It is characterized by the fastest course. As a rule, the process of treatment does not last more than two months. Complications do not usually occur with this form. The prognosis is the most favorable.
- Chronic. As noted above, it develops because of the patients’ negligent attitude toward their health, the immunity of the fungus to medication or improper treatment. Symptoms of candidiasis in its chronic form are blurred. More common in women.
- Persistent. This type of disease is characterized by a subacute course: it appears, and then suddenly goes away. It is difficult to foresee and extremely difficult to treat this form of infection.
- Recurrent. It is characterized by periodic flares, which often become systematic. Can occur with stress or menstruation.
- Carrier state. A person feels great, does not have signs of a yeast infection, but for those around him he is potentially dangerous.
- Candida sepsis. This is the most dangerous and severe form. Fungus can spread throughout the body. It can be found not only on the skin, mucous membranes, but also in the blood. This form of sepsis is difficult to treat. Fatal outcomes were noted.
Classification of Candidiasis (Yeast Infection)
- Oral candidiasis, or thrush, is rarely an issue for healthy children. It may appear on a tongue, the inner surface of cheeks, lips. With more extensive damage- tonsils, palate, and throat are infected. In adults, this type of disease may appear as a result of oral sex with an infected partner.
Oral manifestation of candidiasis. Along with the tongue and lips, the fungus can affect the palate and spread along the respiratory tract - Congenital candidiasis. A woman infects a child during labor or gestation.
- Candidiasis of the skin and nails.
- Urogenital candidiasis. In women, this disease is called vaginal candidiasis or vulvovaginal candidiasis, since it is often manifested by vaginitis and vulvitis.
- Candidiasis of internal organs (visceral).
Yeast Infection Symptoms
Urogenital candidiasis in people of different sex is manifested in different ways. Very often it occurs without any symptoms in women and men and is detected accidentally during medical examination. Sometimes some more obvious symptoms of other genital infections mask the signs of urogenital candidiasis.
Yeast Infection Symptoms in Women
- The first sign of this infection in women is severe itching in the genital area. It leads to scratches, urinary retention and neuroses.
- Burning sensation. Especially it is felt when the patient puts one foot over the thigh of the other in a sitting position. This symptom is a test for candidiasis.
- Creamy white discharge from vagina. The discharge is characterized by a white color and a specific odor (sometimes odorless).
- The genitals become swollen and red.
- Sexual intimacy and urination are accompanied by painful sensations.
All of the above signs may be observed, or it may be no signs at all.
Self-healing is also possible, for example, during menstruation. During this period, the pH level is shifted to the alkaline side. The disease may become chronic. Relapses occur four or more times a year (usually before menstruation). This form of vaginal candidiasis is difficult to treat, the complications are more often observed.
Candidiasis can develop as an independent disease, but is often observed in conjunction with other STDs: chlamydia, ureaplasmosis, trichomoniasis and other infections.
However, the presence of symptoms is not enough to diagnose. A laboratory test is necessary.
Symptoms of Male Candidiasis
In men, the infection is characterized by:
- Redness of the foreskin and head of the penis;
- Severe itching and burning;
- Unpleasant odor;
- Dryness on head of penis;
- Pain during urinating and sexual intercourse;
- The appearance of white deposit on the head of the penis and the foreskin, a white plaque.
Male yeast infection in its protracted form may cause relapses up to 4 times a year and does not manifest itself.
Men who suffer from yeast infection of the genitals are much fewer than women. This is explained by the anatomy of the male genital organs: Candida is easily washed away by urine. The main difference between male and female candidiasis is that in most cases it proceeds in men asymptomatically.
The main way of penetrating the pathogen into the male organism is sexual. Infection in women often occurs because of internal reasons: with intestinal dysbacteriosis or pregnancy.
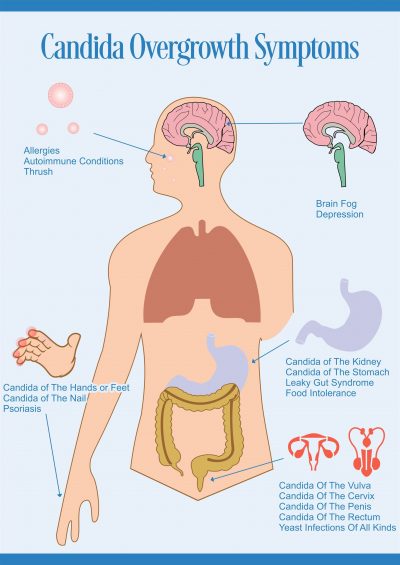
Common Symptoms of Candida Overgrowth

Some Common Symptoms of Candida Overgrowth: Red Rashes, Fever & Chills, Chronic Fatigue, White Discharge from the Genitals, White Layer of Film in the Mouth, Weakness, Itching, Chronic Constipation or Diarrhea, Pain while passing Urine.
| Common Symptoms of Candida Overgrowth | ||
| Metabolic/Digestion Symptoms | Mental/Emotional Symptoms | Whole Body Symptoms |
| Weight gain, obesity | Headaches, migraines | Chronic fatigue |
| Increased belly fat | Sleep problems | Muscle weakness |
| High carbs, sugar, alcohol cravings | Night sweats | Irregular heartbeat |
| Cravings for dairy, sour foods | Lack of concentation | Cold hands & feet |
| Bulimia or anorexia | Mood swings | Allergies, acne, eczema, dandruff |
| Indigestion, acid reflux | Increased irritability | Frequent infections |
| Bloating, gas | High anxiety | Asthma / persistent cough |
| IBS (irritable bowel syndrome) | Hyperactivity / ADD | Itching, running nose / sinus inflammation |
| Hypoglycemia | Memory problems | Ear pain / itching |
| Metabolic syndrome | Brain fog, confusion | Chronic joint pain |
| Thyroid dysfunction | Indecisiveness | Low sex drive / impotence |
| Oral thrush | Sense of floating | Painful intercourse |
| Constipation/diarrhea | Learning disabilities | Fungal infections |
| PMS (pre-menstrual syndrome) | Depression | Rectal / vaginal itching |
Candidiasis Infographics
What are the Causes and Risk Factors of Yeast Infection?
Candidiasis is a very common disease. What are the ways of transmission - let us try to figure it out.
Fungi Candida always exist in the human body. They are on the skin, in the intestines, in the vagina and mouth. Along with a decrease in immunity system, the acidity of the medium changes, resulting in active spreading of the pathogen. The result is an inflammation accompanied by itching, discharge and other signs. That is why even virgins can be infected with genital candidiasis.
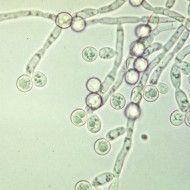
the typical specimen of the Candida fungus
The risk of yeast infection increases when fungi from an infected person in the acute phase of the disease penetrates the body of its sexual partner. It is perfectly possible for both men and women to infect partners with the yeast infection. It should be noted that Candida fungi live in the oral cavity and intestines, so there is a high probability of infection during oral and anal sex.
The organism of a pregnant woman undergoes complex changes. In such conditions, there is high probability of developing vaginal candidiasis. It is dangerous not so much for a woman, as for the fetus. Even without becoming infected during prenatal development, a child runs the risk of getting a thrush after birth.
The main factors that increase the risk of yeast infection are:
- Hypovitaminosis;
- Immunodeficiency of any origin;
- Stress;
- Uncontrolled use of antibiotics;
- Associated STDs;
- Tuberculosis;
- Diabetes;
- Allergies;
- Hormonal changes (for example, during pregnancy).
The emergence of candida infection may be caused by working in warm wet rooms, wearing tight underwear, unsafe hygiene practices.
Consequences of Candidiasis
Urogenital candidiasis is not as dangerous as many other diseases of the genitourinary system. However, it should not be ignored. It is important to conduct therapy in time. This will protect from the "chain" of unpleasant consequences.
Complications arising from chronic yeast infection:
- Yeast infection is more dangerous in pregnant women. Fungi of the genus Candida infect the fetus, which negatively affects the health and even threatens the life of the child.
- Candidiasis can bring disharmony into relationship.
- The spread of candidiasis to the urinary system is not excluded.
How to prevent possible complications? The question is rhetorical - certainly, you should start an adequate treatment in time to get rid of all clinical manifestations.
How is a Vaginal Yeast Infection Diagnosed?
If a patient has only complaints then it is not enough to diagnose. Itching, discharge, pain are observed in a variety of genital diseases. A more accurate reason can be determined by examination and laboratory diagnosis, where specialists may reveal swelling, strong reddening of genitals, erosion, cracks. At this stage of diagnosis, the nature of the infection (bacterial or fungal) and its form (chronic or acute) are assessed.
The laboratory analysis can also aid in diagnosing yeast infections. There are two main methods:
- Cytological examination and a smear on the flora. As a rule, while examining smears stained by Romanovsky’s method a doctor may reveal yeast-like fungi. However, the cytological analysis is not available to every laboratory, but taking smears on the flora is still an excellent diagnostic method, which allows specialists easily find Candida fungi. This method allows you to see the colonies of Candida albicans, as well as pseudomyceliim.
- Bacteriological examination. This method is not very popular, because the cytological analysis of smear is enough to diagnose. The essence of the method is that the material is placed on a special nutrient medium, where an active reproduction of the fungus occurs. As a result, not only the presence of the pathogen is observed, but also its quantity and stage (acute or chronic).
These types of Candida examination methods are used in men. Swelling, reddening of the head of a penis, spots, erosion, plaque are the symptoms of yeast infection. Serological methods and PCR for the diagnosis of yeast infection are practically not used.
Urogenital Candidiasis Treatment
Today more and more people suffer from urogenital candidiasis. This fact may be explained by global changes in lifestyle of modern people all over the world. They keep farther away from nature, does not follow its laws. Stresses, chemical additives in the things they eat and drink, physical inactivity, - weaken our immunity system. The human body is becoming more susceptible without adequate protection. Therefore, the problem of treatment became even more acute.
In addition, the resistance of Candida to medical products is increasing, the therapy turns out to be ineffective in most cases. Another problem is asymptomatic candidiasis. It is becoming more difficult to cure a patient at advanced stage of yeast infection, which does not always lead to complete recovery. Nevertheless, it is necessary to treat any form of yeast infection at any stage of development.
How to Cure Yeast Infection: Therapy and Remedies
The main principle of treatment of candidiasis caused by a pathogenic fungus is the destruction of the pathogen itself. Topical drugs and systemic medication are used. Specialists should choose the best method of treating yeast infection.
Systemic Medication
Depending on the mode of action, the groups are:
- Antifungal antibiotics - nystatin, natamycin;
- Imidazoles - clotrimazole, miconazole, ketoconazole;
- Triazoles - fluconazole, Diflucane, Mycosyst;
- Drugs of different groups - griseofulvin, Nitrofungin, flucytosine and others.
The most effective drugs for the treatment of candidiasis are those, which have fluconazole in the composition. These drugs have many advantages:
- They are well absorbed - up to 90%;
- Do not lead to hormonal problems;
- The time of their use does not depend on the time interval to the last meal;
- Differ by the duration of effect - completely removed from the body in 60 hours.
Nystatin, which was very popular before, now has already lost its relevance due to its poor bioavailability. In addition, the fungi are already well adapted to this drug.
Levorin and amphotericin are considered to be highly toxic and should only be used under experienced medical supervision.
However, other drugs, including fluconazole, can cause complications in different body systems. They have a number of contraindications. Pregnant and breastfeeding women are not allowed to use them at all. In such cases local action drugs (gels, suppositories, vaginal pills, creams) are used.
| Oral (systemic) Candida Albicans Medications | ||
| Drugs (Generics) | Drug class(es) | Medicines (Brand Names) |
| nystatin | mouth and throat products, polyenes | Nystan, Mycostatin, Nystat-Rx, Nilstat, Bio-Statin |
| fluconazole | azole antifungals | Diflucan, Trican, Loitin, Mycosyst |
| clotrimazole | azole antifungals, mouth and throat products | Clotrimazole Troche, Mycelex Troche |
| ketoconazole | azole antifungals | Ketoconazole, Nizoral |
| amphotericin B | polyenes | Fungilin, Abelcet, AmBisome, Fungisome, Amphocil, Amphotec, Fungizone, Amphocin, Fungizone For Tissue Culture |
| terbinafine | miscellaneous antifungals | Lamisil, Terbisil, Zabel, Terbinex |
| itraconazole | azole antifungals | Sporanox, Onmel, Sporanox PulsePak |
| miconazole | azole antifungals | Oravig |
| flucytosine | miscellaneous antifungals | Ancobon |
Topical Remedies
| Topical Candida Albicans Medications | |
| Drugs (Generics) | Medicines (Brand Names) |
| nystatin | Nystop, Mycostatin Topical, Nyamyc, Pediaderm AF, Pedi-Dri, Nystan, Infestat, Nystalocal, Nystamont, Nystex, Mykinac, Nysert, Nystaform, Nilstat, Korostatin, Mycostatin, Mycolog-II, Mytrex, Mykacet, Myco-Triacet II, Flagystatin II, Nyata |
| clotrimazole | Gyne-Lotrimin, Femizole-7, Canesten, MyCelex, Mycelex-7, Agisten, Clotrimaderm, Clotrimazole-Teva, Anti-Fungal Liquid, FungiCURE Pump Spray, Lotrimin AF Cream, Lotrimin Jock Itch Powder, MPM Anti-Fungal, Prescription Strength Cruex |
| ketoconazole | Extina, Ketodan, Kuric, Ketomousse, Nizoral A-D, Nizoral Topical, Xolegel |
| miconazole | Micon 7, Miconazole 3, Monistat, Monistat-Derm, Monistat Vaginal, Monistat 3, Monistat 7, Monistat-1 Day or Night, M-Zole 3, Vagistat-3, Micatin, Daktarin, Gyno-Daktariin, Daktacort, Femizol, Zeasorb-AF, Mitrazol, Aloe Vesta Antifungal, Azolen Tincture, Baza Antifungal, Carrington Antifungal |
| econazole | Econazole Nitrate, Ecoza, Spectazole Topical |
| ciclopirox | Ciclodan, Ciclodan Kit, CNL8 Nail, Loprox, Pedipirox-4, Penlac Nail Lacquer, Loprox TS |
| tioconazole | Vagistat-1, Monistat-1 |
Topical drugs are divided into:
- One-component - e.g. suppositories with miconazole, clotrimazole;
- Multicomponent - for example: Tergynan, Polygynax, clion-D. These drugs affect not only Candida fungi but some other pathogens too.
Special antifunginal sprays may take strong effect on the main signs of candidiasis, eliminating itching, burning and inflammation; stimulates the increase in number of lactobacilli, prevents the risk of relapses. It is recommended to use systemic action drugs simultaneously.
The advantages of topical drugs:
- The minimum of contraindications;
- The active substance affect the place of pathogen accumulation;
- Does not affect the liver and kidneys;
- Relatively safe for pregnant women.
Despite the advantages of topical drugs, many experts suppose using them is not enough for an adequate treatment. They believe that creams and ointments act only on fungi, which are localized in the uppermost layers of the skin. However, Candida spores located deeper are not available for them. The treatment should be carried out in a complex way - both by topical and systemic medications.
In addition to direct exposure to the fungus, additional measures should be taken to prevent its reproduction:
- Normalize the immune system. This can be done with the help of immunomodulating drugs, for example, isoprinosine. Take them in accordance with the package leaflet. Firstly, doctors must examine the state of the patient's immunity.
- Normalize metabolic processes in the body. It is noticed that candidiasis often occurs in people with a metabolic disorder. Such patients can be recognized by obesity, diabetes, thyroid problems. It can be concluded that reduction in weight and blood sugar, restoring the proper functioning of the thyroid gland facilitates more effective treatment of urogenital candidiasis.
- Adjusting the Diet. Diet is an important step for the successful treatment. What are the conditions, which lead to the turbulent activity of baker's yeast? In an environment rich in carbohydrates! The yeast fungus of the genus Candida acts on the same principle. Goodies, sweets, sweet drinks - a paradise for the pathogen. The main principle of nutrition is cutting down on sweets and rich fermented goods. Eat more vegetables, cereals and fruits.
Methods for the Prevention of Urogenital Candidiasis
Most experts agree on the following preventive principles:
- Syringing should be avoided. Even during menstruation and after sexual intercourse. Keep the external genitals clean. Syringing can disrupt the balance of bacteria in the vagina and can alter the normal pH of the vagina.
- The external genitalia should be kept clean. Do not use ordinary soap for intimate hygiene. It is better to use clean water.
- Use condoms.
- If you have to take antibiotics, you should eat sour-milk products containing lactobacilli, or medicinal preparations.
- Do not use deodorants, foams, powders, bleaches very often; they can negatively affect the microflora of genitals.
- Do not wear tight clothing, especially underwear, as it can cause inflammation of the genitals.
- The underwear should "breathe". It should be made of cotton fabrics.
- It is necessary to keep the genitals dry. After swimming, you need to change clothes, and wash a swimsuit.
- Do not use hygienic tampons. It is better to replace them with pads.
- Monitor the blood sugar level.
If you have symptoms of candidiasis - even with several symptoms, you should immediately contact a doctor and undergo treatment. Yeast infection is not a shameful venereal disease. It occurs for a number of reasons. Sexual contact is only one of them. Do not blame your sexual partner.
 include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Less commonly the penis may be affected, resulting in itchiness. Very rarely, the infection may become invasive, spreading to other parts of the body.
include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Less commonly the penis may be affected, resulting in itchiness. Very rarely, the infection may become invasive, spreading to other parts of the body.