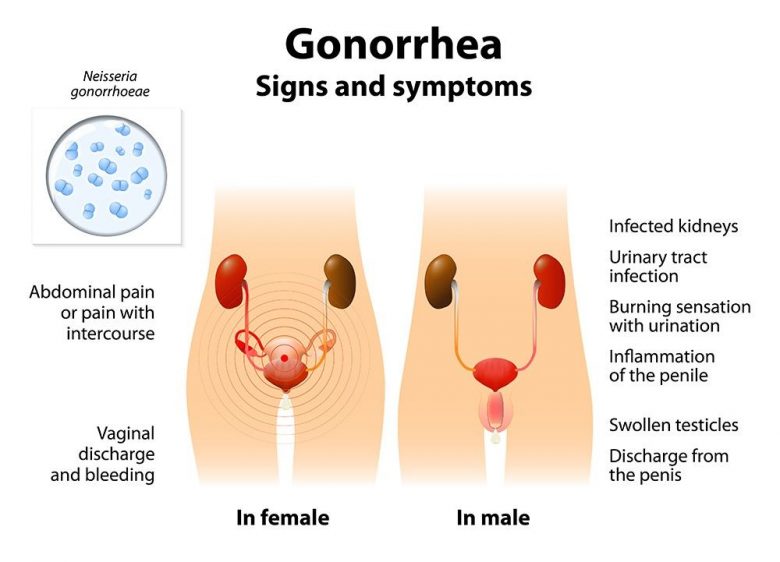
Gonorrhea is a sexually transmitted infectious disease caused by gonococcus (Latin Neisseria gonorrhoeae), characterized by the damage to mucous membranes of the genitals and organs of the urinary system. It is transmitted mainly during sexual intercourse. Gonorrhea affects not only the mucous membranes of the genital tract (in most cases), but the mucous membrane of the rectum, conjunctiva, oropharynx can be also affected. In this article you can learn more about the ways of infection, symptoms of gonorrhea in men and women, prevention, treatment, and antibiotics.

Contents
- 1 What is Gonorrhea?
- 2 Neisseria Gonorrhoeae Photos
- 3 Getting Infected with Gonorrhea
- 4 Is Gonorrhea Transmitted through a Kiss?
- 5 Is Gonorrhea Transmitted through a Condom?
- 6 Gonococcal Infection in the Newborn
- 7 Symptoms of Gonorrhea
- 8 Symptoms of Gonorrhea in Women
- 9 Symptoms of Gonorrhea in Men
- 10 Diagnostics
- 11 Treatment of Gonorrhea
- 12 Antibiotics for Gonorrhea
- 13 The Most Popular Medications for Uncomplicated Gonococcal Infection Treatment
- 14 Prevention of Gonorrhea
- 15 Complications
What is Gonorrhea?
Gonorrhea is a sexually transmitted disease that causes damage to the mucous membranes of organs lined with cylindrical epithelium: urethra, uterus, rectum, pharynx, conjunctiva of eyes. The pathogen is gonococcus.
Gonococci quickly die in special conditions (when heated, dried, treated with antiseptics or in direct sunlight). Gonococci mainly affect the mucous membranes of organs with cylindrical and glandular epithelium. They can be located on the surface of cells and intracellularly (in leukocytes, trichomonads, epithelial cells), can form L-forms (not sensitive to the effects of drugs and antibodies).
 Gonorrhea is characterized by mucous and purulent discharge from the urethra or vagina, pain and discomfort during urination, itching and discharge from the anus. If the pharynx is affected, a throat and tonsils are inflamed. Untreated gonorrhea in women and men causes inflammation of the pelvic organs, leading to infertility; Gonorrhea in pregnant women leads to infection of a child during childbirth.
Gonorrhea is characterized by mucous and purulent discharge from the urethra or vagina, pain and discomfort during urination, itching and discharge from the anus. If the pharynx is affected, a throat and tonsils are inflamed. Untreated gonorrhea in women and men causes inflammation of the pelvic organs, leading to infertility; Gonorrhea in pregnant women leads to infection of a child during childbirth.
Several types of gonococcal infection are distinguished by the location of lesion:
- gonorrhea of the urogenital organs;
- gonorrhea of the anorectal region (gonococcal proctitis);
- gonorrhea of the musculoskeletal system (gonarthritis);
- gonococcal conjunctival infection of the eyes (blenorrhea);
- gonococcal pharyngitis.
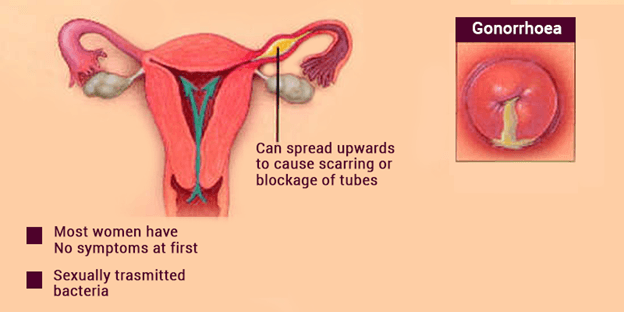
Gonorrhea from the lower parts of the genitourinary system (urethra, periurethral glands, cervical canal) can spread to the upper (uterus and appendages, peritoneum). Gonorrheic vaginitis almost does not occur, since the flat epithelium of the vaginal mucosa is resistant to the effects of gonococci.

Gonorrhea is more common among young people 20 - 30 years old, but can occur at any age. The danger of complications of gonorrhea is very high - various genitourinary disorders (including sexual disorders), infertility in men and women. Gonococci can penetrate the blood. Circulating throughout the body they can cause damage to joints, sometimes gonococcal endocarditis and meningitis, bacteremia, severe septic conditions.
With some symptoms of gonorrhea, which are difficult to spot, patients aggravate the course of their illness and spread the infection further without knowing it.
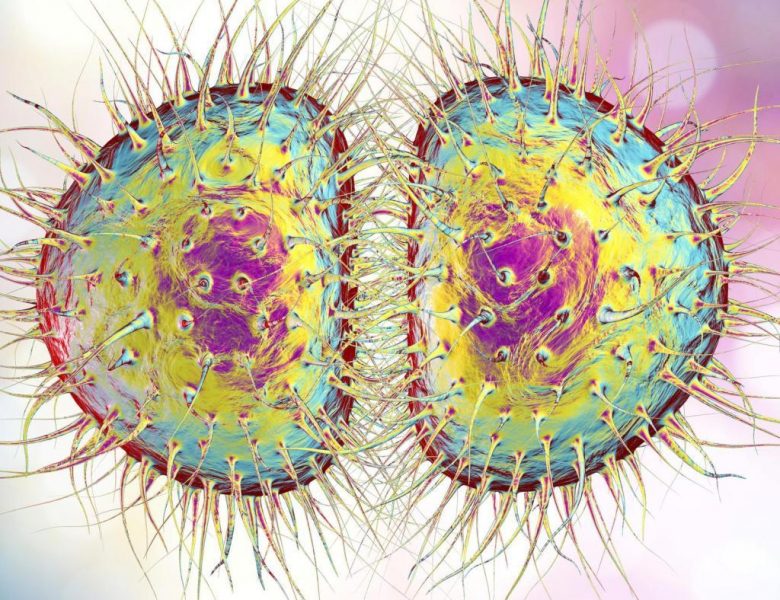
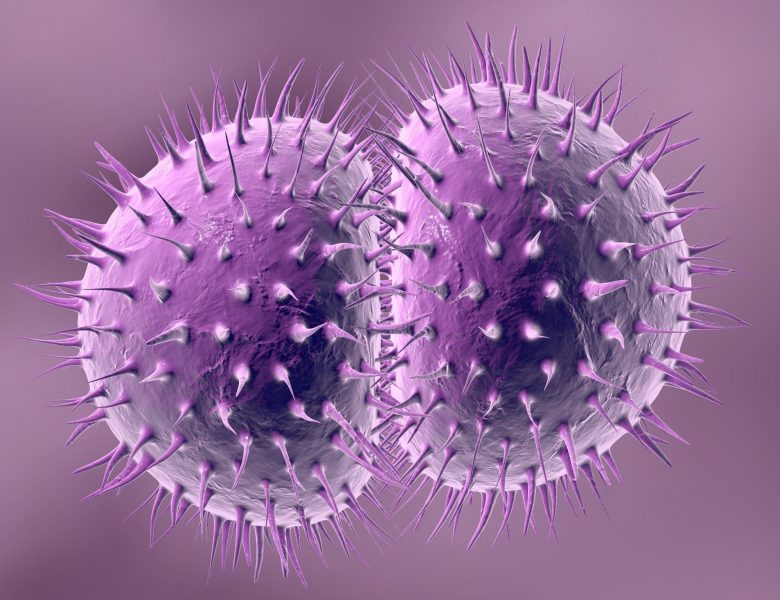
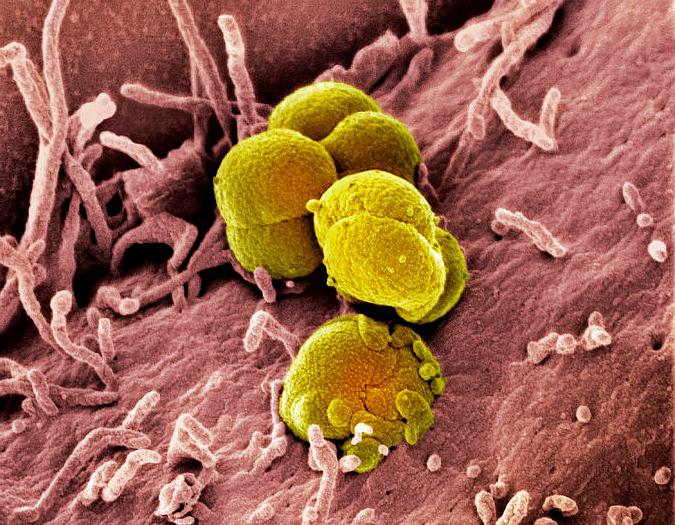
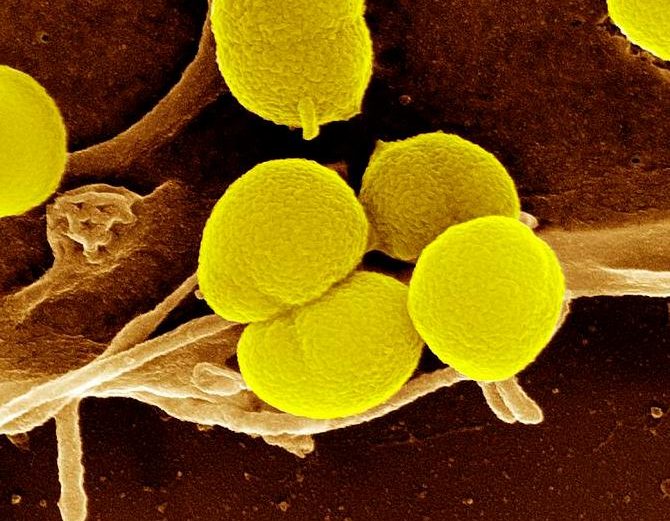
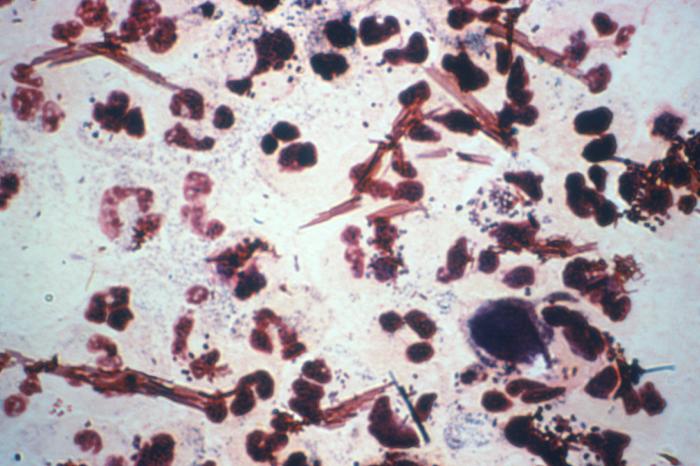
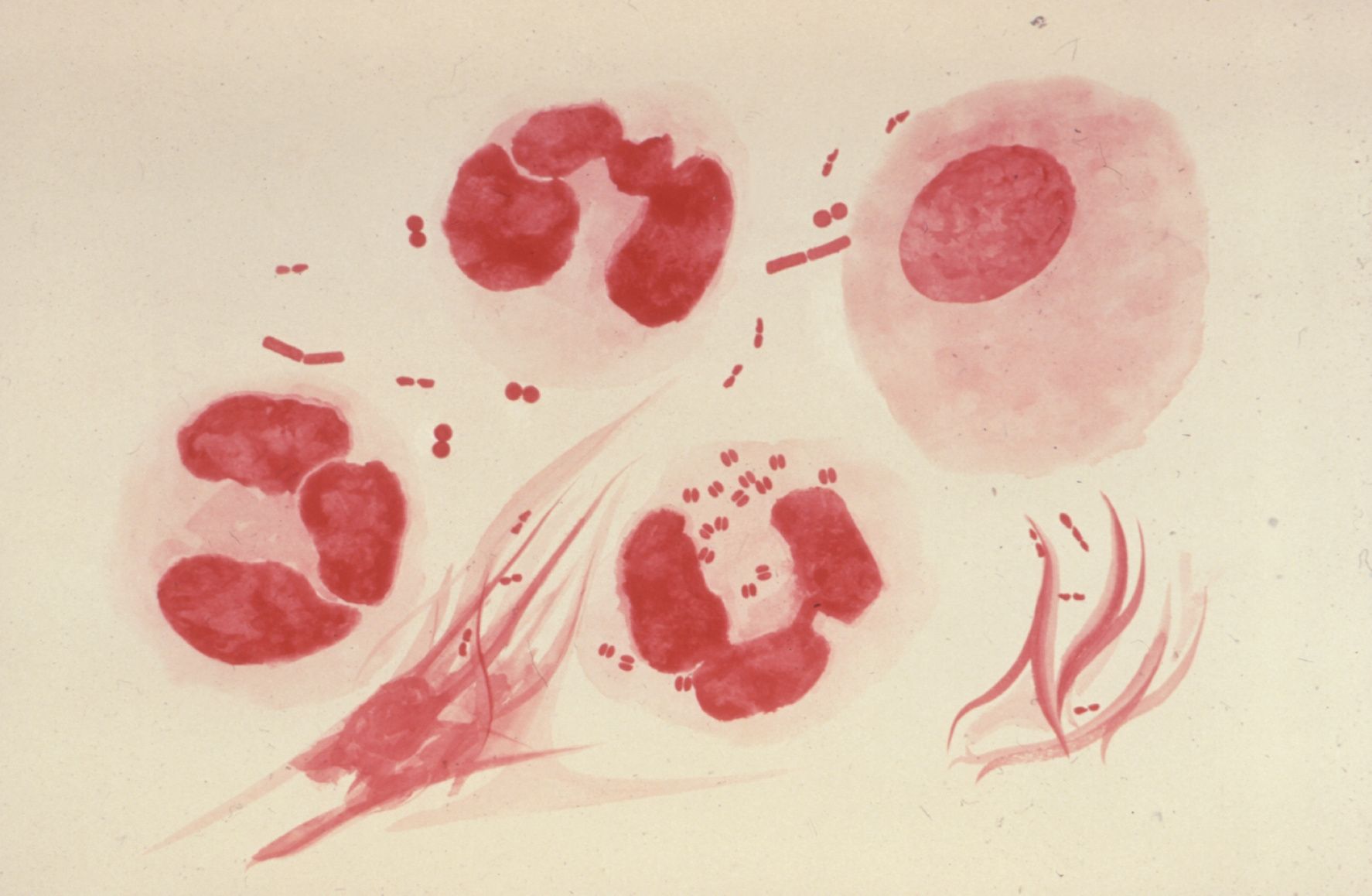
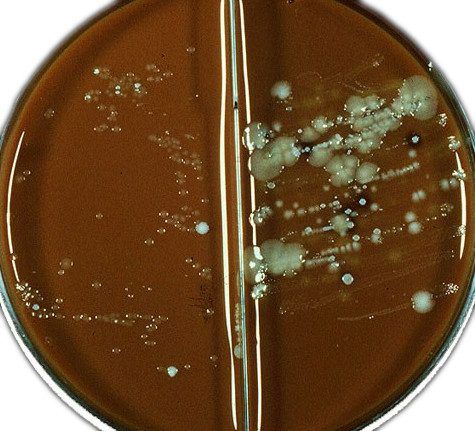
Neisseria Gonorrhoeae Photos
Pictures (click →)


Getting Infected with Gonorrhea
Gonorrhea is a highly contagious infection, in 99% has a sexual way of transmission. Infection with gonorrhea occurs with different forms of sexual contact: vaginal, anal and oral.
The probability of being infected with gonorrhea in women after sexual intercourse with an infected man is 50-80%. Men who have sex with infected women do not always get infected (30-40% of cases). This is due to some anatomical and functional features of the urogenital system in men (the narrow canal of the urethra, gonococci can be washed away by urine.) The probability of being infected is higher if a woman has menstruation and the sexual intercourse is lengthened.
Sometimes there may be a contact way of infection of a child from an infected woman, and indirect - through personal hygiene items (bed linen, towels), usually in girls.
The incubation period of gonorrhea can last from 1 day to 2 weeks, less often up to 1 month.
Is Gonorrhea Transmitted through a Kiss?
 Gonococcal infection is most often localized in the urethra and on the mucous membrane of the genital organs. In this case, the transmission of the disease through a kiss is impossible, since there is no causative agent in the oral cavity or in saliva. However, there are also atypical forms of this disease, in which other organs and systems are affected. One of such forms is pharyngeal gonorrhea or gonococcal pharyngitis.
Gonococcal infection is most often localized in the urethra and on the mucous membrane of the genital organs. In this case, the transmission of the disease through a kiss is impossible, since there is no causative agent in the oral cavity or in saliva. However, there are also atypical forms of this disease, in which other organs and systems are affected. One of such forms is pharyngeal gonorrhea or gonococcal pharyngitis.
During this disease gonococci colonize the mucous membrane of the pharynx and, more rarely, the oral cavity. Then it is theoretically possible to transmit the pathogen to the partner while kissing. However, the chance of becoming infected in this case is extremely small.
Transmission of pharyngeal gonorrhea through a kiss is unlikely for the following reasons:
- Gonococci in the throat are in unusual conditions. The mucous membrane of the urethra is best for their reproduction, which differs in structure from the mucous membrane of the mouth and pharynx. Because of this, the number of gonococci is smaller and the probability of infection decreases.
- Human immunity also plays a significant role in this form of gonorrhea. The probability of infection is higher, if the patient's immunity is weakened. In this case, the body struggles badly with the microbe, and the gonococci become more active.
- The mucous membrane of the pharynx is better suited for gonococci than the oral cavity.
Thus, the risk of infection with gonorrhea through a kiss is extremely small. To transfer the infection to the mucous membrane of the other person's mouth, too many conditions must be observed. In the so-called "social" kiss (not mouth to mouth) when there is no direct exchange of fluids, gonorrhea can not be transmitted at all. Even a large number of pathogens on skin will quickly die. A healthy skin barrier is impenetrable for gonococci.
Is Gonorrhea Transmitted through a Condom?
 Condoms are the most simple and affordable way to protect yourself from sexually transmitted diseases. There are many researches proving that condoms are effective against all bacterial and most viral infections. Gonococci, which cause gonorrhea are bacteria. They have a relatively large size (compared, for example, with viruses) and are unable to penetrate the microscopic pores of the latex from which the condom is made. Thus, it can be argued that gonorrhea is not transmitted through a condom.
Condoms are the most simple and affordable way to protect yourself from sexually transmitted diseases. There are many researches proving that condoms are effective against all bacterial and most viral infections. Gonococci, which cause gonorrhea are bacteria. They have a relatively large size (compared, for example, with viruses) and are unable to penetrate the microscopic pores of the latex from which the condom is made. Thus, it can be argued that gonorrhea is not transmitted through a condom.
Nevertheless, there are two important exceptions, which need to be taken into account. First, condoms are highly effective in protecting from gonorrhea only when they are used correctly. In most cases, people who were infected through a condom simply could not properly use them.
To achieve a maximum protection against infection, the following rules must be observed:
- Compliance with the expiration date. On each package of condoms the expiration date is indicated. If it is exceeded, the lubricant inside begins to dry out, and the latex loses its elasticity; the risk of its burst increases during an intercourse. Even if the condom does not tear, it will have microcracks, which are larger than normal pores. Gonococci can penetrate through them.
- Use every time you have sexual contact. Gonococci can affect not only the mucous membrane of the urinary tract, but also other tissues (albeit with less probability). Therefore, the condom should also be used for orogenital and anogenital contact. However, in these cases the risk of its burst increases to 3-7%.
- Correct opening of the package. Not every condom package can be easily opened by hands. To do this, it is necessary to tear it from the side of the ribbed surface. Opening the package with sharp objects (knives, scissors) or teeth can lead to accidental latex damage.
- Put it on properly. When putting on a condom, the penis should be in an erection state. Otherwise, it can slip off and form folds, and in the process of sexual intercourse the risk of burst will increase.
- Air release. Pinch the end of the condom when you put it on to leave space for the sperm. This end is designed to collect sperm after ejaculation. If you do not release the air in advance, the risk of a burst is high.
- Use a condom for each act of intercourse or when you change the type of intercourse during the same encounter. The condom should be worn even during a foreplay. After the sexual intercourse, wrap the condom in paper tissue and throw it in the garbage, wash the penis with warm water to remove the sperm remnants.
The second important point, explaining the possibility of infection with gonorrhea is that condoms are protected only from the transmission of gonococcal infection localized in the urethra. It is this area that is protected by latex during sexual intercourse. However, there are a number of other gonorrhea forms.
Gonococcal Infection in the Newborn
Gonococci can not penetrate intact membranes during pregnancy, but premature rupture of these membranes leads to infection of amniotic fluid and fetus. Gonococcal infection in the newborn can occur when it passes through the birth canal of an infected mother. The conjunctiva of the eyes and genital organs are affected. Blindness in newborns in half cases is caused by gonorrhea infection.
Symptoms of Gonorrhea
Based on the duration of the disease, fresh gonorrhea (from the moment of infection <2 months) and chronic gonorrhea (from the moment of infection >2 months) are distinguished.
Fresh gonorrhea can take place in acute, subacute, malosymptomatic (torpid) forms. Gonorrhea does not always have the typical clinical symptoms, since a mixed infection (with Trichomonas, Chlamydiae), which can change symptoms, lengthen the incubation period, make it difficult to diagnose and treat the disease. There are many low-symptom and asymptomatic cases of gonorrhea.
Gonococcal pharyngitis can be manifested by redness and pain in the throat, an increase in body temperature, but more often it is asymptomatic. With gonococcal proctitis, discharge from the rectum can be observed, tenderness in the anus, especially during defecation.
Chronic gonorrhea is prolonged, manifested by adhesive processes in the small pelvis, decreased sexual desire in men, menstrual irregularities and reproductive function in women.
Symptoms of Gonorrhea in Women
Classical manifestations of the acute form of gonorrhea in women:
- purulent vaginal discharge;
- hyperemia, edema and ulceration of mucous membranes;
- frequent and painful urination, burning, itching;
- intermenstrual bleeding;
- lower abdominal pain.
In more than half of cases, gonorrhea in women is either lethargic, low-symptomatic. Gonorrhea affects the uterus, fallopian tubes, ovaries and peritoneum. The general health condition may worsen, the body temperature may rise (up to 39 ° C), there is a violation of the menstrual cycle, diarrhea, nausea, vomiting.
In girls gonorrhea is manifested by edema and hyperemia of the vulvar mucosa and vestibule of vagina, burning and itching of the genitals, purulent discharge, pain during urination.
Symptoms of Gonorrhea in Men
Gonorrhea in men is mainly in the form of acute urethritis:
- itching, burning, swelling of the urethra;
- abundant purulent discharge;
- frequent painful, sometimes difficult urination.
With the ascending type of gonorrhea the testicles, prostate, seminal vesicles are affected, the body temperature rises, a painful defecation are observed.
Diagnostics

For the diagnosis of gonorrhea clinical symptoms are not enough, it is necessary to identify the causative agent of the disease using laboratory methods:
- microscopic examination of the discharge from the urethra after painting a special dye discharge;
- methods of collection of clinical specimens on specific growth media to determine clear culture;
- ELISA and PCR diagnostics.
In the microscopy of smears stained with Gram and methylene blue, the gonococci are determined by being bean-shaped and paired, gram-negative and by intracellular position. The causative agent of gonorrhea can not always be detected by this method because of its variability.
When diagnosing asymptomatic forms of gonorrhea, as well as in children and pregnant women, a more appropriate method is the culture method (its accuracy is 90-100%). The use of selective medium (blood agar) in addition to antibiotics can accurately detect even a small number of gonococci and their sensitivity to drugs.
The material for research on gonorrhea is purulent discharge from the cervical canal (in women), the urethra, the lower part of the rectum, the oropharynx, the conjunctiva of the eyes. Girls and women after 60 years of age use only the culture method.
Gonorrhea often occurs as a mixed infection. A patient with gonorrhea is examined additionally for other STIs, HIV, serological reactions to syphilis, general and biochemical analysis of blood and urine, ultrasound of the pelvic organs, urethroscopy, in women - colposcopy, cytology of the mucous cervical canal.
Surveys are conducted before the beginning of treatment, repeatedly after 7-10 days of treatment, serological - in 3-6-9 months.
Treatment of Gonorrhea

Self-treatment of gonorrhea is inadmissible, it is fraught with transmission of the disease into a chronic form, and the development of irreversible damage to the body. All sexual partners of patients with gonorrhea symptoms who had sexual intercourse with them for the last 14 days, or the last sexual partner are subject to examination and treatment. In the absence of clinical symptoms a patient with gonorrhea is examined, all sexual partners must be treated.
For the period of gonorrhea treatment alcohol, sexual relations are excluded, during the period of dispensary observation sex is not recommended even with the use of condoms.
Antibiotics for Gonorrhea
 Modern venereology has in its arsenal many effective antibacterial drugs that can successfully fight gonorrhea. The treatment of gonorrhea takes into account the prescription of the disease, the symptoms, the location of lesion, the absence or presence of complications, concomitant infection. With an acute ascending type of gonorrhea, hospitalization, bed rest, medical treatment are necessary. In the event of purulent abscesses (salpingitis, pelvioperitonitis), an emergency surgery is performed - laparoscopy or laparotomy. Antibiotic therapy is one of the most frequently used methods of treatment. However the resistance of some gonococcal strains to antibiotics should be taken into account (for example, penicillins). If the antibiotic is ineffective, another drug is prescribed.
Modern venereology has in its arsenal many effective antibacterial drugs that can successfully fight gonorrhea. The treatment of gonorrhea takes into account the prescription of the disease, the symptoms, the location of lesion, the absence or presence of complications, concomitant infection. With an acute ascending type of gonorrhea, hospitalization, bed rest, medical treatment are necessary. In the event of purulent abscesses (salpingitis, pelvioperitonitis), an emergency surgery is performed - laparoscopy or laparotomy. Antibiotic therapy is one of the most frequently used methods of treatment. However the resistance of some gonococcal strains to antibiotics should be taken into account (for example, penicillins). If the antibiotic is ineffective, another drug is prescribed.
Gonorrhea of the genitourinary system is treated with the following antibiotics: ceftriaxone, azithromycin, cefixime, ciprofloxacin, spectinomycin. Alternative regimens for treating gonorrhea include the use of ofloxacin, cefosidime, kanamycin (in case of absence of hearing disorders), amoxicillin, trimethoprim.
 Ceftriaxone 250 mg intramuscularly, with azithromycin 1 g orally once or with doxycycline 100 mg twice a day - 7 days (the safest form - doxycycline monohydrate) - is the preferred therapy for uncomplicated gonococcal infections of the cervix, urethra and rectum. Both azithromycin and doxycycline can be used in treatment of gonorrhea, and combination therapy can delay resistance to a certain type of antibiotics. Thus, the combination therapy is recommended even if there is no suspicion of co-infection with Chlamydia trachomatis or co-infection is excluded.
Ceftriaxone 250 mg intramuscularly, with azithromycin 1 g orally once or with doxycycline 100 mg twice a day - 7 days (the safest form - doxycycline monohydrate) - is the preferred therapy for uncomplicated gonococcal infections of the cervix, urethra and rectum. Both azithromycin and doxycycline can be used in treatment of gonorrhea, and combination therapy can delay resistance to a certain type of antibiotics. Thus, the combination therapy is recommended even if there is no suspicion of co-infection with Chlamydia trachomatis or co-infection is excluded.
Doxycycline is most effective in treatment of Chlamydial urethritis in men.
The information in this article is provided for informational purposes only and should not be used for self-management.
Drugs for Gonorrhea Treatment:
- Azithromycin

This is a broad-spectrum antibiotic, based on erythromycin. In comparison with erythromycin, azithromycin takes many advantages. Unlike the alternative antibiotics of the macrolide group, azithromycin as a representative of the subclass of azalides, is rapidly absorbed, acid-fast and eliminates gonococcus from the body much faster.
According to some reports, no gonococcus is detected within 24 hours after taking the drug. The persistence of azithromycin in therapeutic concentrations is noted directly in the inflamed area within a week after the last reception. Azithromycin makes it possible to affect the most resistant strains.
A single dose of azithramycin increases the patient's compliance, simplifies the treatment and increases the effectiveness of the therapy. 1-2 grams once are taken in acute gonorrhea, or 1 g in 2 doses. It is taken before meals. Sometimes intravenous drugs can be used. 1 gram is prescribed in case of chronic gonorrhea, followed by 250 mg every day for 4 days. Dosage should be adequate. With the simultaneous detection of C. trachomatis, azithromycin is given orally at a dosage of 1 g, which increases the effectiveness of combination therapy.
The drug does not interact with the cytochrome P 450 system, which is why it can be combined with other antimicrobial agents. The results of several studies confirm that in acute gonorrhea 1 g of the drug increases the effectiveness of treatment to 90-93%. With increasing the dose up to 2 g, it rises to 99%, but the risk of gastrointestinal side effects also increases.
For gonorrhea of pharynx this antibiotic is less effective.
Azithromycin is not prescribed for the treatment of gonorrhea in pregnant women and children. Mainly because of possible side effects (diarrhea, increased level of liver enzymes).
- Ceftriaxone

- Doxycycline

To treat gonorrhea, doxycycline is used. For seven days one capsule (100 mg) is required twice a day. Complex use of metronidazole (2 tablets) 2 times a day. The scheme of treatment is individual, it is assigned by a specialist based on analyzes. Self-treatment is inadmissible - this can lead to complications.
500 mg of antibiotic are used in case of uncomplicated urethritis. 300 mg at first and 100 mg every 6 hours twice.
With a complicated form of the disease, 900 mg are used, dividing the dose into 6 doses. In case of chronic form, the course of antibiotics should be increased to 14 days. The optimal option is 1 pill every 12 hours.
Doxycycline in gonorrhea is used immediately after a meal, with plenty of water.
Doxycycline like most antibiotics has unpleasant side effects, which can include nausea, skin rash, dizziness and sweating. With prolonged use of doxycycline dysbacteriosis, thrush and discoloration of the teeth are possible.
Contraindications. The drug is contraindicated in pregnant women and during lactation, in children at the age of 9 years, in case of acute hepatic or renal insufficiency, leukopenia.
After doxycycline treatment of gonorrhea the solarium and direct sunlight are contraindicated for 5 days.
- Erythromycin – This antibiotic is only used as medicine for gonorrhea for babies who have contracted the STD during birth from an infected mother.

Fluoroquinolones are contraindicated to children up to 14 years; tetracyclines, fluoroquinolones, aminoglycosides to pregnant women and nursing mothers. Antibiotics that do not affect the fetus (ceftriaxone, spectinomycin, erythromycin); that can be used for preventive treatment of newborns (ceftriaxone - intramuscularly, rinsing with a solution of silver nitrate or applying of erythromycin ophthalmic ointment to eyes).
Treatment of gonorrhea can be adjusted in case of a mixed infection. In torpid, chronic and asymptomatic forms of gonorrhea, it is important to combine the main treatment with immunotherapy, local treatment and physiotherapy.
Local treatment of gonorrhea includes rinsing vagina, urethra with 1-2% solution protorgol, 0.5% solution of silver nitrate, microclysters with chamomile extract. Physiotherapy (electrophoresis, UFO, UHF currents, magnetotherapy, laser therapy) is used in the absence of an acute inflammatory process. Immunotherapy with gonorrhea is used to enhance immune responses and is divided into a specific (gonorrhea vaccine) and nonspecific (pirogenal, autohaemotherapy, prodigiozan, levamiozol, methyluracil, glyceryl, et al.). Immunotherapy is not carried out in children under 3 years old. After treatment with antibiotics, lacto- and bifidopreparations are prescribed (oral and intravaginal).
The successful outcome of gonorrhea treatment is the disappearing of the symptoms and the absence of a pathogen according to the results of laboratory tests (7-10 days after the end of treatment).
Currently, the need for numerous control examinations after the end of gonorrhea treatment conducted by modern highly effective antibacterial drugs is disputed. One visit to doctor is recommended to determine the adequacy of treatment. Laboratory control is prescribed if there are some clinical symptoms, symptomatic relapse of the disease or repeated infection.
The Most Popular Medications for Uncomplicated Gonococcal Infection Treatment
| azithromycin |
| ceftriaxone |
| ciprofloxacin |
| cefixime |
| doxycycline |
| levofloxacin |
| cefuroxime |
| tetracycline |
Prevention of Gonorrhea
Prevention of gonorrhea, like other STDs, includes:
- personal prophylaxis (exclusion of casual sexual relations, use of condoms, observance of rules of personal hygiene);
- prompt detection and treatment of gonorrhea patients;
- medical examinations (children's institutions, medical personnel, food workers);
- mandatory examination of pregnant women and pregnancy management.
In order to prevent gonorrhea, a solution of sodium sulfacyl is injected into the eyes immediately after the birth.

Complications
Asymptomatic cases of gonorrhea are rarely detected at an early stage, which contributes to the further spread of the disease and gives a high percentage of complications.

Ascending type of infection in women with gonorrhea is promoted by menstruation, surgical termination of pregnancy, diagnostic procedures (scraping, biopsy, sounding) and intrauterine device insertion. Gonorrhea affects the uterus, fallopian tubes, ovarian tissue until the onset of abscesses. This leads to a violation of the menstrual cycle, the emergence of adhesions in the tubes, the development of infertility, ectopic pregnancy. If a woman with gonorrhea is pregnant, there is a high probability of spontaneous miscarriage, premature birth, infection of the newborn and development of septic conditions after childbirth. Newborns infected with gonorrhea have an inflammation of the conjunctiva of eyes, which can lead to blindness.
A serious complication of gonorrhea in men is gonococcal epididymitis, a violation of spermatogenesis, a decrease in the ability of spermatozoa to fertilize.
Gonorrhea can pass to the bladder, ureters and kidneys, pharynx and rectum, affect lymph glands, joints, and other internal organs.
If you start treatment in time, adhere strictly to the prescription of a venereologist and lead a healthy lifestyle you can avoid unwanted complications of gonorrhea.