
Contents
- 1 What Is Molluscum Contagiosum?
- 2 What Are the Symptoms?
- 3 Pictures
- 4 What Are the Causes?
- 5 How Does Molluscum Contagiosum Spread?
- 6 What Are the Risk Factors for Contracting an Infection?
- 7 How Is the Virus Diagnosed?
- 8 What Are the Treatment Options?
- 9 Are There Any Home Remedies?
- 10 What Is the Outlook for Molluscum Contagiosum?
- 11 How Can Molluscum Contagiosum Be Prevented?
- 12 Frequently Asked Questions
What Is Molluscum Contagiosum?
As a viral skin infection, molluscum contagiosum causes benign lesions or raised bumps on the top layers of the skin. The bumps are round, firm and range in size, but they do not usually cause pain. In most cases, they go away on their own without leaving scars. However, scratching them can make the infection spread, and scars may develop from open lesions.
The time that it takes for the virus to run its course varies between people, but it can take two months to four years. Treatment is available from general physicians or dermatologists for bumps that do not disappear or for people who want to have them removed.
Molluscum contagiosum most commonly occurs in children age 1 to 10 years, but adults can be infected too, especially if their immune systems are weak. When adults with healthy immune systems have the genital virus, doctors tend to categorize it as a sexually transmitted infection.

Names: Molluscum Contagiosum (MC), Water Warts, Molluscum Contagiosum Virus (MCV)
What Are the Symptoms?
The symptoms of molluscum contagiosum might not manifest for up to six months after infection. On average, though, the incubation period is two to seven weeks. Then, between one and 30 bumps will appear. Their characteristics usually include
- firm, dome- or pear-like shape;
- dimple or dent in the center;
- 2 to 5 millimeters in diameter;
- itchy, smooth and shiny;
- pink, red, white or flesh-colored;
- yellow or white waxy core; and
- cracked, red skin around them.
The lesions often affect the torso, arms, legs, neck and face. However, they can develop on the inner thigh and genital areas as well. They do not appear on the soles of feet or palms of hands.
People with weak immune systems could have bumps as large as 15 millimeters. They also tend to have more lesions on their faces and be more resistant to treatment.
Pictures
What Are the Causes?
The cause of molluscum contagiosum is a virus of the same name that can survive on surfaces such as
- skin,
- clothes,
- towels,
- tools,
- pool equipment, and
- sports gear.
When people touch these infected surfaces, they can contract the infection. Squeezing, scraping or scratching the bumps can also spread the virus.
How Does Molluscum Contagiosum Spread?
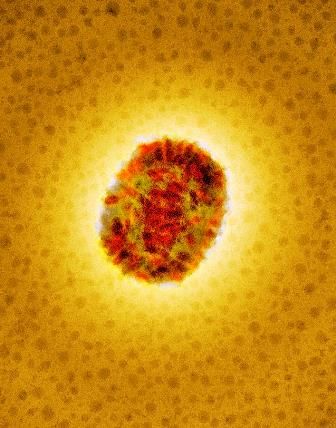
Molluscum Contagiosum Virus (MCV). Coloured transmission electron micrograph of MCV.
The molluscum contagiosum virus can spread through direct, physical contact with infected persons or inanimate objects. It has not been proven whether or not the virus can be spread through warm, wet environments such as baths, saunas and swimming pools.
People who scratch or touch one of their own bumps could spread the virus by touching other parts of their bodies. This process is called autoinoculation, which can occur through electrolysis and shaving too. Sexual contact can also spread molluscum contagiosum when people come into direct contact with the virus. Although not all adult cases of the infection occur this way, many of them do.
However, it is unclear if the lesions have to be broken or open for the virus to transmit between people. Researchers have determined, though, that the infection remains in the epidermis, which is the top of layer of skin. For that reason, it does not circulate in the body and cannot spread by sneezing or coughing.
Unlike herpes viruses, molluscum contagiosum does not remain dormant in the body and redevelop. Once the lesions disappear, the virus is cured and cannot spread to others.
What Are the Risk Factors for Contracting an Infection?
People should not be surprised if they see someone with molluscum contagiosum or become infected because it is pretty common. However, some people have a higher risk for contracting the virus than others:
- Atopic dermatitis could be a risk factor for developing the infection because it involves frequent skin breakage. Because of that, people who have this condition are likely to transmit the virus to other parts of their bodies.
- People who live in crowded living conditions in humid, warm climates may have an increased risk for spreading and contracting the infection.
- People with weak immune systems from cancer treatments or HIV, for instance, have a higher risk than those with healthy immune systems. They could also have larger outbreaks and be less receptive to treatment.
- Playing contact sports such as football and wrestling might increase the risk because they involve skin-to-skin contact.
How Is the Virus Diagnosed?
The distinct appearance of molluscum contagiosum lesions makes the virus easy for doctors to diagnose. However, they can also resemble chicken pox, skin cancer and warts.
Although treatment is usually not necessary for molluscum contagiosum, it is important to see a doctor for skin conditions that last longer than a few days to rule out worse problems. To do that, physicians can perform a biopsy or scraping to analyze the skin under a microscope.
What Are the Treatment Options?
Most of the time, molluscum contagiosum gets better in six to 12 months without seeking treatment. However, it is common for people to want to remove visible bumps for appearance purposes and to prevent further transmission.
In some cases, treatment is necessary because of underlying conditions such as atopic dermatitis or because the lesions are on the genitals. Also, the occurrence of genital molluscum contagiosum could indicate the presence of another sexually transmitted disease that requires medical attention.
It is important to understand that some treatments are painful, so general physicians or dermatologists may use anesthetics beforehand. They might also use a combination of methods to cure the infection. Once the bumps are gone, the virus is also gone and no longer contagious. However, treating the infection does not make people immune to getting it again.
Physical Removal
Doctors can use a few different methods to physically remove molluscum contagiosum lesions. Some people have irritation, pain and scarring afterward. These methods are fast and might require local anesthesia:
- Cryotherapy is a treatment that involves using liquid nitrogen to freeze the bumps. The physician applies the nitrogen directly to the infected area, which destroys the skin lesions.
- A curette might also be used to remove the bumps. The physician applies pressure to the surgical instrument and uses a scraping motion to pierce and remove the lesions.
- A doctor could use laser therapy, which involves applying a laser to each bump.
When a curette or laser is used, people might need more than one treatment session to get rid of the bumps. They may also need additional treatment every three to six weeks if the bumps are large. The treatment will continue until the infection is completely gone.
Oral Therapy
Oral treatments are a less painful solution to physical removal. For that reason, they are the more popular choice for treating children. They also allow parents to complete the treatment in a more comfortable environment at home.
Oral cimetidine is a histamine-receptor antagonist that children can tolerate, and it is safe and painless. However, molluscum contagiosum bumps that are on the face do not respond as well to this treatment as lesions that appear elsewhere.
Topical Therapy
Sometimes, doctors prescribe topical medications to treat molluscum contagiosum. While these medications are safe, many of them are not recommended for use during pregnancy:
- adapalene,
- cantharidin,
- imiquimod,
- iodine and salicylic acid,
- potassium hydroxide,
- tazarotene,
- topical podophyllotoxin cream,
- tretinoin, and
- trichloroacetic acid.
Potassium hydroxide is the active ingredient in MolluDab, the most recommended topical medication for molluscum contagiosum. The cream is dotted on the lesions twice a day to break down the viral skin cells so that the immune system can fight the infection.
Once the immune system produces an inflammatory response, the skin can heal. This treatment method takes two to six weeks. Like other topical remedies, MolluDab does not cause the pain or potential scarring that is associated with physical removal.
Therapy for People With Impaired Immune Systems
The above treatment options and topical medications are usually effective for people who have healthy immune systems. However, those whose immune systems are weak because of a disease such as HIV or cancer treatments do not always have the same success.
Instead, treatments that boost the immune system are the most effective methods for these immunocompromised individuals. Antiretroviral therapy, for instance, is effective for those with HIV. Intralesional interferon therapy is a less desirable but effective method because of side effects such as depression, lethargy, site tenderness and flu-like symptoms.
Are There Any Home Remedies?
It is possible to treat molluscum contagiosum with home remedies from ingredients that you might have in your kitchen. Medicinal herbs and essential oils may also be effective. However, anyone who attempts to use these remedies must talk to a doctor first:
- Apple Cider Vinegar – The antiviral and antibacterial traits in apple cider vinegar make it a suitable molluscum contagiosum remedy. Use a cotton ball to dab the infected areas, and let the skin dry before washing it with warm water. Repeat two or three times a day.
- Baking Soda – This common baking ingredient has antioxidant qualities. Mix 2 to 3 teaspoons in water, and heat it for 20 to 25 minutes. Apply the mixture to the lesions with a cotton cloth for about 10 to 15 minutes a day to fight the virus.
- Coconut Oil – With antiviral, antibacterial and antifungal properties, coconut oil can treat many skin problems. After applying it to the bumps, it reduces itchiness and heals the infection.
- Garlic – This common cooking herb has properties that boost the immune system to help the body fight molluscum contagiosum. Cut it into small pieces, and cover them on the bumps with bandages.
- Neem – This medicinal herb is an antiviral substance and widely used to treat viruses. Simply boil the leaves in water, and apply the mixture to the lesions.
- Oregano Oil – Containing antioxidant compounds such as rosmarinic acid and thymol, oregano oil boosts the immune system to fight the virus. Blend three or four drops of this essential oil with a few drops of coconut oil. Using a cotton cloth, apply the mixture to the bumps once or twice a day.
What Is the Outlook for Molluscum Contagiosum?
Molluscum contagiosum usually goes away in six to 12 months for people who have healthy immune systems. It could take a few months to four years for the virus to disappear in those with weak immune systems.
The most common complication is a secondary bacterial infection. It can be a major problem for people with weak immune systems and require antibiotics. Bumps that occur near the eyes could cause a conjunctivitis or keratitis infection that makes the eyes sensitive to light and sore.
Scarring is another possible complication. This happens when people scratch or pick at the lesions. It is also more likely when people have the bumps physically removed.
Once the bumps fade, the virus is no longer present in the body, so it can no longer spread to other body parts or people. Unlike getting chicken pox, though, having the virus once does not protect against getting it again. More lesions can develop if the body becomes infected again.
How Can Molluscum Contagiosum Be Prevented?
The best method to avoid molluscum contagiosum is to not touch the infected skin of someone else or an infected surface. Having good hygiene habits and following viral prevention techniques can also keep the infection from spreading:
- wash hands with soap and warm water to remove germs;
- do not share clothing, goggles, hairbrushes, sports equipment, towels and other personal items;
- avoid swimming without watertight bandages;
- do not pick at, scratch or touch the bumps;
- avoid using electrolysis or shaving over the lesions;
- keep the affected areas clean and covered with bandages or clothing; and
- do not engage in sexual activity when molluscum contagiosum bumps are on or near the anus, penis, vagina or vulva.
Frequently Asked Questions
Is Molluscum Contagiosum a Viral Infection?
Yes, it is a viral infection. In adults, it is categorized as a sexually transmitted infection when the virus spreads during sexual activity.
Some doctors might refer to it as genital molluscum contagiosum. This simply means that the virus appears on or near the genitals after sexual contact. It is prudent to talk to a doctor if bumps or lesions appear on or around the anus, penis, vagina or vulva.
How Does Molluscum Contagiosum Develop?
Molluscum contagiosum goes through three phases. The first stage is when the lesions start to appear. They often develop in clusters and may be hard to see under normal light.
The second phase is contagious. The lesions grow into pearly bumps, and some of them develop indents with pus-filled heads. In general, the more pus-filled heads that there are, the longer that it will take to treat the virus.
During the third stage, the pus-filled heads burst, changing the appearance of the bumps to raised spots. At this point, the infection peaks and triggers inflammation in surrounding skin. It also increases the likelihood of the infection spreading to other parts of the body.
Can Molluscum Contagiosum Be Cured?
This virus is curable with various treatments or medications that doctors can apply or prescribe. The most popular treatment is MolluDab, a topical cream. However, other topical creams, gels or liquids are available. The virus can also be physically removed via cryotherapy, curettage and laser therapy. Oral therapy and home remedies may be effective too.
Once the infection is cured, it can no longer be spread. However, the body can become infected again if it comes into contact with the virus.













