
Contents
- 1 What is Chlamydia?
- 2 The Causative Agent of Infection is Chlamydia Trachomatis
- 3 Causes of Chlamydial Infections
- 4 Ways of Infection
- 5 Microbiological Features of Chlamydia Trachomatis
- 6 Clinical Manifestations and Symptoms of Chlamydia
- 7 Symptoms of Chlamydia in Women
- 8 Symptoms of Chlamydia in Men
- 9 Symptoms of Oral Chlamydia
- 10 Complications
- 11 Chlamydia Tests. Diagnosis of Chlamydia Trachomatis Infection.
- 12 Chlamydia Treatment
- 13 Drugs and Antibiotics for Chlamydia Trachomatis
- 14 List of Chlamydia Infection Drugs
- 15 Prevention of Chlamydia
What is Chlamydia?
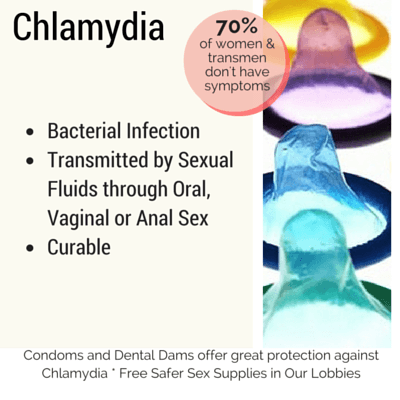
Chlamydia is a sexually transmitted infection caused by microorganisms called Chlamydia trachomatis. It is one of the most common sexually transmitted diseases.
According to statistics, 100 million people become infected with chlamydia every year. At a conservative estimate, the number of people infected with chlamydia around the globe is about one billion. The wide spread of chlamydial infection is associated primarily with the asymptomatic course of the disease.
Chlamydia is referred to non-gonococcal inflammatory diseases of the urogenital system. Compared to gonorrhea, the incubation period is longer, the clinical manifestations are less pronounced, complications occur very often. The infertility is a common outcome of the disease.
The Causative Agent of Infection is Chlamydia Trachomatis
Chlamydia, unlike many other microorganisms, can damage both the external and internal genital organs, the mucosa of the respiratory tract, the intima of vessels and heart, the synovial lining of joints, teeth, and the sense organs.
Chlamydia trachomatis is a Gram-negative obligate intracellular bacterium. Chlamydial infection affects mainly the genitourinary system. Nowadays urogenital chlamydia is the most common cause of non-gonococcal urethritis (up to 60%). Being hidden during a long period of time, chlamydia are able to transform into so-called L-forms – and to "hibernate”. This phenomenon contributes to long intracellular parasitism without conflicts with the host's immune system. In the process of cells’ division chlamydia trachomatis are transferred to daughter cells. Active reproduction and so-called “awakening” of chlamydia from L-forms is possible only during the process of immunosuppression.
Chlamydia trachomatis is divided into the following antigenic serotypes:
- A, B, Ba, C - cause trachoma;
- D, E, F, G, H, I.J, K - cause conjunctivitis and urogenital infections;
- L1, L2, L3 - cause the venereal lymphogranuloma.
Barely discernible in light microscopes Chlamydia trachomatis did not attract the close attention of scientists before, because they had neither an anamnestic record nor a noisy history of its discovery. Chlamydia microorganisms could not be classified as viruses or bacteria, because they function more complicated than the first, but easier than the second.
Earlier they were given the following names: Miyagawanella, Halprowia, Bedsonia.
Causes of Chlamydial Infections
Chlamydia is characterized by asymptomatic or mild symptoms, high contagiosity.
Chlamydia microorganisms cause the inflammation of joints (arthritis), conjunctivitis and inflammation of lungs. Up to about 50% of all diagnosed prostatic inflammations are Chlamydial.
Up to 85% of chlamydia infections are combined with other venereal diseases (gonorrhea, syphilis, trichomoniasis, ureaplasmosis and mycoplasmosis).
Such combinations are more difficult to treat and they are far harder on patients: higher intoxication, complications in the form of infertility and purulent inflammatory urogenital processes.
Ways of Infection
Infection with chlamydiosis is usually sexually transmitted. But while gonorrhea can be transmitted during sexual intercourse to 3 out of 4 people, only 1 out of 4 can be infected with Chlamydia. Women are more susceptible to chlamydia.
The incubation period is from 2 weeks to 1 month. The main ways of infection are vaginal or anal sexual intercourse, household contacts (sauna, bath).
Children can become infected while passing through the birth canal of a woman infected with chlamydiosis. A household way of transmission can occur from contaminated hands to eyes and genitals. Chlamydia microorganisms remain infective on household items up to 2 days at a temperature of 19-20 degrees in wet conditions.
Microbiological Features of Chlamydia Trachomatis
- Intracellular parasitizing - combines chlamydia trachomatis with viruses. They are unable to synthesize ATP and completely depend on the energy resources of the cell and destroy it completely in the process of parasitizing.
- The presence of the cell membrane - combines chlamydia with bacteria - makes it possible to use antibiotics for treatment.
- A unique life cycle. Chlamydia are characterized by a very special life cycle, which begins with the infection of sensitive host cells through a chlamydia-specific process of phagocytosis.
Chlamydia exist in the body in two forms:
- Elementary corpuscle or extracellular infectious bodies.
- Reticular bodies - intracellular form of pathogen.
Scientists were unable to classify Chlamydia for a long period of time, because these microorganisms combine both the characteristics of viruses and bacteria.
Learn more about viruses:
Being completely intracellular bacterium Chlamydia resembles a virus: it depends on the nutrients and energy of the host cell, does not synthesize ATP. But like all other bacteria it contains both DNA and RNA and multiplies by division.
Clinical Manifestations and Symptoms of Chlamydia
Chlamydia is very often asymptomatic, with minimal manifestations. It follows in 46% of men and 70% of women absolutely without symptoms. If the symptoms are present, they are not pronounced clearly.
Symptoms of Chlamydia in Women
Chlamydia in women manifests itself by such symptoms as vaginal discharge mucous or mucopurulent. They can be characterized by an unpleasant odor or a yellowish tinge. Chlamydia microbes can infect the urethra and cause a urinary tract infection, which can manifest itself in pain during urination (most commonly a 'burning' sensation). Abdominal, lower back pain or a heavy feeling around the hips, bleeding between periods. In addition, women may have general weakness and elevated temperature - symptoms of intoxication.
Symptoms of Chlamydia in Men
In men, the symptoms of chlamydial infection appear in most cases as a mild inflammation of urethra of a protracted (chronic) course - urethritis, which lasts at least several months. Men may have white watery discharge from the urethra. Most of men complain about burning and itching at the opening of the urethra. There may be different pains, mostly not violent: it can hurt in the urethra, in the scrotum, in the lower back, in the testicles. The temperature can rise up to 37 degrees; a man can feel a general weakness - a consequence of intoxication. There may be a clouding of urine, the presence of purulent threads in it.
In a number of cases, there is a long-term preservation of chlamydia in the body in the form of isolated microcolonies on the mucous membranes. With clinical, instrumental and laboratory examination no signs of organ damage are detected - a person is clinically healthy, and only with the use of high-precision methods of laboratory diagnosis (PCR) chlamydia can be detected. This condition is associated with the suppression of chlamydia reproduction by the body's immune system.
Symptoms of Oral Chlamydia
This type of symptoms is not necessarily associated with infection through sexual intercourse (including oral). It is possible to be infected through utensils and wounds in the mouth. With an oral chlamydiosis the patient experiences nasal congestion. Thick sticky mucus can be found in the nasopharynx. This mucus has a very unpleasant smell, which resembles a rotten fish. In most cases, it forms small areas and then grows on the entire oral cavity.
The mucus has a white color. The tonsils and the back of the throat begin to swell. If you press a little on soft tissues in the oral cavity, the patient experiences pain. Hyperemia is not observed. Gradually the patient loses the sensitivity of the receptors of the tongue because of the specific coating. Then it will be very difficult to chew and swallow food due to the pain. The mucus accumulates under the root of the tongue. The patient will feel as if he/she has many abrasions in the mouth and the trachea. Epithelial layers of the tongue will gradually dry, crack and peel off. Breathing will have a very unpleasant smell. In some cases, there is involuntary twitching of the tongue, which is caused by spasms.
Asthmatic seizures are also possible, and it is difficult for a patient to breathe in air as well as exhale. It becomes difficult to breathe at night; eosinophils are increased. The manifestation of only one of the symptoms is possible, which makes diagnosis more difficult. Patients with similar symptoms should be checked for chlamydial infection.
Complications
Urogenital complications of chlamydia in men are chlamydial prostatitis, urethritis, epididymitis.
- prostatitis develops when the prostate gland is involved in the infection process. Chlamydial prostatitis is accompanied by unpleasant sensations and pains in the lower back, rectum, perineum, slight mucous or watery discharge from the urethra, difficulties with urinating;
- urethritis proceeds with urethral tract infection and is characterized by itching, frequent painful urge to urinate, mucopurulent discharge. Chronic urethritis caused by chlamydia leads to urethral stricture;
- epididymitis develops with inflammation of the epididymis, which is accompanied by high fever, swelling and reddening of the scrotum, an increase in the epididymis.
Urogenital complications of chlamydiosis are fraught for men with a violation of spermatogenesis and infertility.
Chlamydia in women causes various lesions of the reproductive system. Chlamydial infection in genital tract can cause inflammatory changes in:
- uterine cervix - endocervicitis. Chlamydia increases the risk of developing tumors;
- the mucous membrane of the uterine cavity - endometritis;
- Fallopian (uterine) tubes - salpingitis;
- uterine appendages - salpingoophoritis.
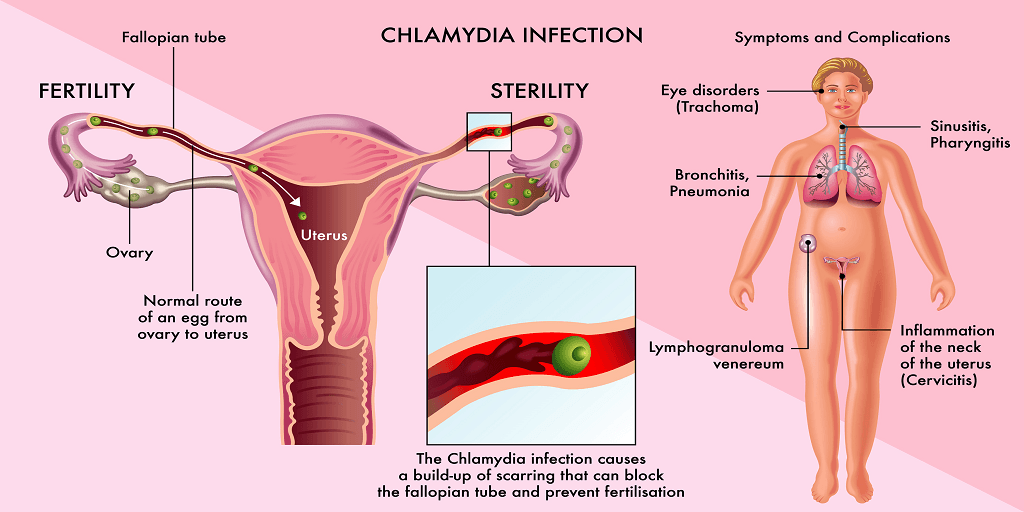
Inflammatory processes in the uterus and uterine appendages with the subsequent formation of adhesions and scars in the uterine tubes are the cause of infertility, ectopic pregnancy and spontaneous abortion.
Other effects of chlamydia in men and women are the inflammatory processes of pharynx, rectum, kidneys, joints, lungs, bronchi, etc. One of the serious complications of chlamydia is Reiter's disease, characterized by the following clinical manifestations: conjunctivitis, urethritis, arthritis. Repeated infection with chlamydia significantly increases the risk of complications.
The congenital chlamydia is the most dangerous form of disease. The main forms of congenital chlamydia are:
- chlamydial conjunctivitis (ophthalmocamidiosis) - inflammation of the mucous membrane of eyes;
- generalized form of chlamydia – the damage of heart, lungs, liver, digestive tract;
- encephalopathy accompanied by convulsions and respiratory arrest;
- Chlamydia pneumonia is an extremely severe form of pneumonia with a high mortality rate.
Chlamydia Tests. Diagnosis of Chlamydia Trachomatis Infection.
The diagnosis of chlamydia is complex, because Chlamydia trachomatis is an intracellular parasite. In this regard, neither smears (mucus and discharge) nor scrapings (cells of the diseased organ) are not taken for the diagnosis of chlamydia. Non-invasive tests are sometimes more acceptable for patients. The material for analysis on chlamydia can also be blood, urine and sperm.

The following laboratory methods are used to detect chlamydia:
- Polymerase chain reaction (PCR). The results of this analysis will be ready in a day or two. This method gives false results only in the event of violations in the process of sampling, transportation or analysis of biomaterials. Confirmation of a positive result obtained by PCR is not required. This method is recommended as the preferred method for the diagnosis of Chlamydia infection.
- Sowing on chlamydia. Of all the methods of diagnosing chlamydia, this is the most expensive method - the results of the analysis are ready after several days. However, these shortcomings are more than compensated: if the analysis on chlamydia by the method of inoculation gives a positive result, there can be no doubt that these bacteria are in the patient’s body. The main advantage of this analysis is the possibility of determination of antibiotics, which can be used for treatment. This method reveals chlamydia in 70-90% of cases.
The other diagnostic methods have a low level of reliability, and according to some clinical researches, they cannot be recommended for detecting chlamydial infection. Pharmacy tests (so-called home chlamydia tests) are accurate in only 20% of cases, enzyme immunoassay (ELISA) in 60%, immunofluorescence (RIF) - 50%, and microscopic analysis - only 15%. All the results should be confirmed by PCR analysis.
Chlamydia Treatment
The treatment is aimed at destroying the pathogen, eliminating inflammation, preventing the complications of chlamydia.
Since Chlamydia trachomatis is an intracellular parasite, the choice of drugs is limited to those that are able to penetrate into the cell.
Drugs and Antibiotics for Chlamydia Trachomatis
In accordance with the latest international standards (WHO recommendations, European recommendations 2010 – European guideline for the management of Chlamydia trachomatis infections), the most effective drug for urogenital chlamydia is azithromycin - a single dose; or a 7-day course of doxycycline is used.
Treatment of uncomplicated chlamydiosis includes:
- azithromycin for infections of the urogenital tract caused by Chlamydia trachomatis (urethritis, Cervicitis). For the treatment of uncomplicated urethritis / cervicitis it is prescribed in a single dose of 1000 mg (1 g).
or
- doxycycline (100 mg twice a day for at least 7 days).
Medications containing azithromycin. Brand names: Zithromax, Azithromycin Dose Pack, Z-Pak, Zmax.
Medications containing doxycycline. Brand names: Vibramycin, Oracea, Adoxa, Monodox.
You are probably interested in the following question "how soon can I have sex again?"
If you had a one-day course of azithromycin, you should avoid sex at least for a week after the treatment.
Alternative drugs are other macrolides and fluoroquinolones. The safety profile allows pregnant women to use azithromycin (B category by FDA). Other macrolides are not recommended for pregnancy (C-category).
In addition to antibiotics, the scheme of chlamydia treatment sometimes includes antifungal drugs (fluconazole), immunomodulators (interferon). In case of abundant secretions from the urethra, local antimicrobial agents are also used.
In some cases, additional treatment is prescribed (immunotherapy, prostate massage, urethral instillation, physiotherapy, etc.).
In case of chronic chlamydia (especially if it is complicated), antibiotic therapy is longer and often combined (several antibiotics are used).
All partners who were in sexual contact with a patient must be necessarily checked. During the period of treatment, the sexual activity is not recommended, alcoholic drinks are prohibited. It is also recommended to limit the use of dairy products.
After 6-9 weeks after the end of the treatment the patient should carry out PCR again (the results must be negative).
List of Chlamydia Infection Drugs
| Medications Used to Treat Chlamydia Infection |
| doxycycline |
| azithromycin |
| amoxicillin |
| erythromycin |
| tetracycline |
| levofloxacin |
Prevention of Chlamydia
Prevention of chlamydia is aimed at preventing infection with chlamydia, identifying the carriers and all sexual partners who have been in contact with the patient.
To prevent the ways of chlamydia can spread means to protect sexual relations, to exclude favorable conditions for everyday infection or infection of a child during pregnancy and childbirth.
Chlamydia is an infection that is easier to avoid than to get rid of it. The main rules for preventing chlamydia, as well as other sexual infections, are:
- having a permanent sexual partner. The best prevention of urogenital chlamydia is to have a sexual intercourse with one partner.
- avoiding casual sex;
- using condoms;
- examination for infections if there was an unprotected sexual intercourse;
- notification of all sexual partners in case of confirmation of the chlamydia diagnosis;
- examination of women who are planning pregnancy for hidden infections (including chlamydia) and careful management of pregnancy. Before planning the pregnancy women should do all the necessary diagnostic tests for chlamydia. It is important to make sure that both parents are healthy.
- abstinence from sexual intercourse during the treatment. The sexual intercourse cannot be completely safe, even if using a condom, vaginal suppositories or douches with antiseptics.
The spreading of chlamydia through household items can be avoided by following simple rules of individual hygiene. Do not use other people's toothbrushes, unwashed linen or towels and always wash your hands thoroughly before the intercourse.
The general measure of prevention Chlamydia is a health promotion. The correct diet, seasonal intake of vitamins and physical exercises will increase the susceptibility to chlamydia.
This information is provided for informational purposes only and should not be used for self-treatment.




